Chest Physiotherapy Nursing Interventions
Steering Group
Julia Bott (Chair), Support to Section 6, Consultant Therapist, Surrey PCT NW
Sheric Ellum provides support for Section 5, consultant physiotherapist Guy’s and St Thomas’ NHS Trust in London
Dr Rachel Garrod, support to Section 1, Reader, School of Physiotherapy, Faculty of Health and Social Care Sciences, Kingston University and St George’s, University of London.
Support to Sections 3, 4 and 5, Dr Jennifer Pryor Senior Research Fellow in Physiotherapy at Royal Brompton & Harefield NHS Trust
Dr Lesley Rimington supports Section 2 Lecturer School of Health and Rehabilitation at Keele University
Thoracic Mobility Exercises
Level of evidence 2-
Research recommendation
- This patient group should continue to research the effects of thoracic mobility exercise on vital capacity, lung capacity, and clinical outcomes.
- Further research into the use of thoracic mobility exercises and their effects on vital capacity, total lung capacity and clinical outcome should be undertaken in this patient group.
This patient group should continue to research the effects of thoracic mobility exercise on vital capacity, lung capacity, and clinical outcomes.

Nasal cannulae
Most patients tolerate the nasal cannulae (Fig 1 attached). They do not need to be removed when the patient is talking or eating. Oxygen is inhaled even when breathing through the mouth. Useful nasal cannulae:
- Stable patients
- Supplemental oxygen therapy for meals
- To provide air-driven nebulised therapy for those requiring controlled oxygen therapy.
They are commonly used to deliver oxygen in the home setting.
High flow rates of more than 4L/min may cause significant drying of the nasal mucosa. This can make it harder to bear. Patients with uncontrolled type 2 respiration should avoid nasal cannulae because the FiO2 they achieve varies depending on how deep and fast they breathe.
Maximal Insufflation Capacity
Recommendations
- When oxygen saturation falls below 95% the use of non-invasive ventilation and/or strategies to aid airway clearance should be considered. (Grade D)
If oxygen saturation drops below 95%, it is worth considering non-invasive ventilation or strategies that aid in airway clearing. (Grade D)
- Use some form of maximal insufflation strategy to improve effective cough generation when vital capacity falls below 1500 ml or 50% predicted. (Grade D)
If vital capacity is below 1500ml, or the predicted 50%, you can use a maximal insufflation strategy. (Grade D)
- Patients with bulbar dysfunction, who cannot breathe stacks, should be given single maximum insufflation. (Grade D)
Use single maximal insufflation techniques for patients with bulbar dysfunction who are unable to breath stack. (Grade D)
- Teaching patients with no bulbar muscle involvement how to do unaided breathing stacking on their own. (Grade D)
Teach patients without bulbar muscle involvement unaided breath stacking to improve cough effectiveness independently where possible. (Grade D)
- Regular breath stacking (10-15 times three times per day) to maximal insufflation capacity should be performed by patients with vital capacity of less than 2000 ml or 50% predicted. (Grade D)
Patients with a vital capacity less than 2000ml, or 50% of predicted capacity, should perform regular breath stacking (between 10-15 times per day), to maximize insufflation. (Grade D)
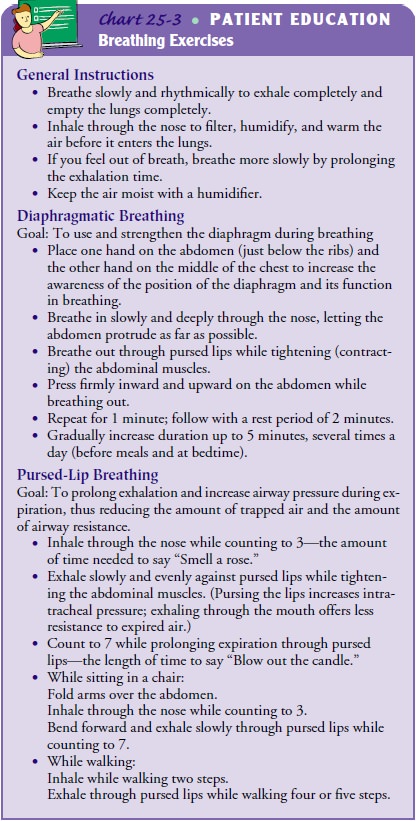
Exhalation On Effort (“Blow As You Go!”)
When the shoulder girdle moves, the ventilation load falls on the diaphragm. This is something that many people with COPD or hyperinflation have difficulty with.23 The upper limb activities often exacerbate dyspnoea. Moreover, the effort of inhalation creates a respiratory load in its own right. It is possible for patients to have an inclination to hold their breath during exertion. This can be counterproductive. This technique is aimed at avoiding both breath-holding and inhaling with effort. When the patient raises their arms high above their heads, bends down or is stretching, they are instructed to exhale.
Level of evidence 4
Recommendation
- As a strategy for reducing dyspnoea among patients suffering from COPD, you might teach exhalation on effort (or “blow as your go!”). (Grade D)
- Teach exhalation on effort (“blow as you go!”) as a potential strategy to reduce dyspnoea in patients with COPD. (Grade D)
As a strategy for reducing dyspnoea among patients suffering from COPD, you might teach exhalation on effort (or “blow as your go!”). (Grade D)
It’s a good point
- It is strongly advised to avoid holding your breath during exercise.
- Breath-holding during exertion should be strongly discouraged.
Breath-holding during exertion should be strongly discouraged.
The Goals and Outcomes
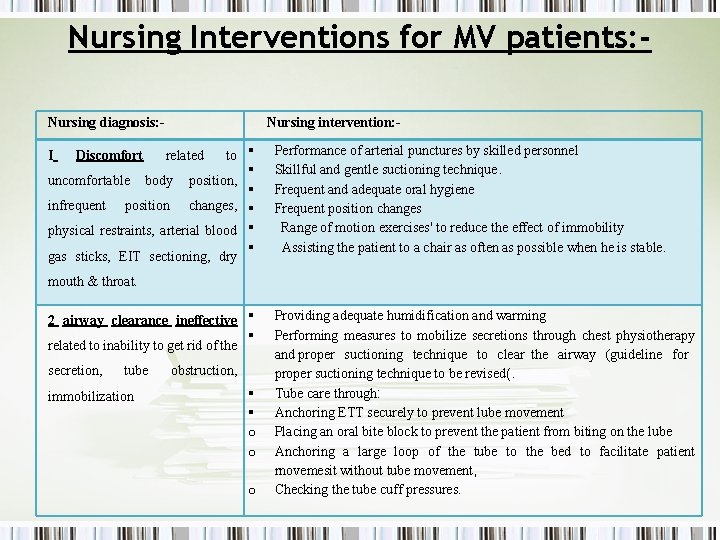
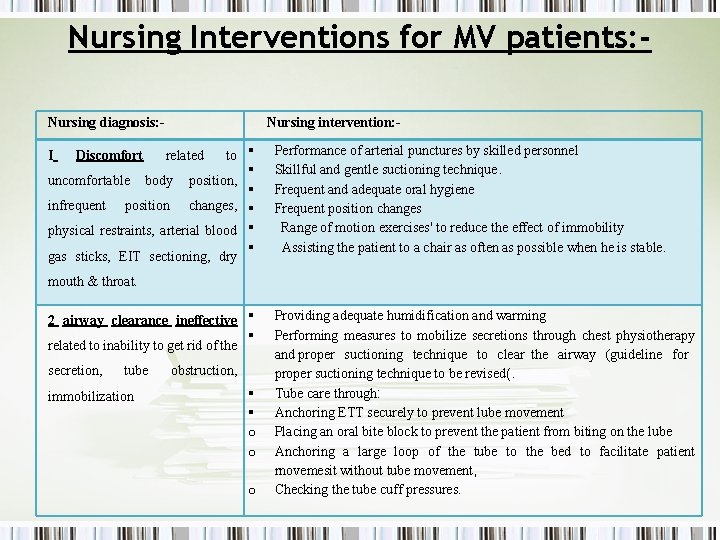
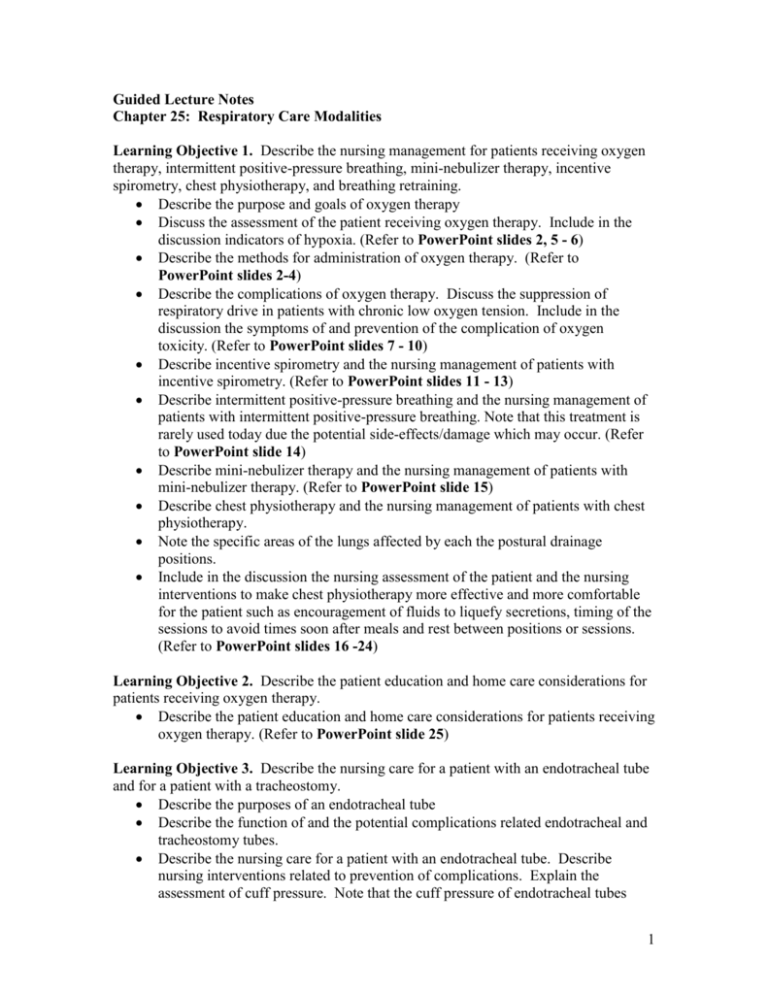
These are the goals and outcomes that Ineffective Clearance will achieve.
- Patient will maintain clear, open airways as evidence by normal breath sounds, normal rate and depth of respirations, and ability to effectively cough up secretions after treatments and deep breaths.
- Patients will show increased air exchange.
- Patient will classify methods to enhance secretion removal.
- Patients will be able to recognize changes in the sputum, including color, character and amount.
- Patient will identify and avoid specific factors that inhibit effective airway clearance.
Nurse Assessment for Ineffective Clearance of Airways
Continuous assessment is necessary in order to know possible problems that may have lead to Ineffective Airway Clearance as well as name any concerns that may occur during nursing care.
- Decreased or absent breath sounds
- Wheezing
- Crackles with coarse salt
- Bronchospasm
- Expiratory grunt
- Rales
- Rhonchi
- Stridor
- Wheeze
- Apnea
- Apneusis
- Ataxic patterns
- Biot’s respiration
- Bradypnea
- Cheyne Stokes respiration
- Eupnea
- Hyperventilation
- Kussmauls respirations
- Tachypnea
Endurance training
Despite heterogeneity of training and assessment methods across included studies, all demonstrated an improvement in endurance with training. The only long-term study372 demonstrated increases in respiratory muscle strength and endurance up to 10 months after commencement of respiratory muscle training in DMD and SMA subjects, at which point the effects stabilised, although the increases in strength and VC were maintained for the whole 3-year training period. This suggests a reduction in the expected VC decline in this patient group and could therefore potentially help delay the commencement of respiratory support.
364 training the respiratory muscles resulted in an increase in strength and endurance, according to a small controlled study. In another small study, in patients with postpoliomyelitis,366 a subjective improvement in the capacity to perform activities of daily living and increased perception of well-being were reported post-training. However, it should be noted that these improvements could have been due to some learning effects from the respiratory muscle strength tests.
Evidence Level 2
Despite the poor methodological quality, these papers show consistent trends in improved lung strength and endurance after respiratory muscle training. Recent physiological evidence indicates that the protection mechanism for nitric dioxide release in exercise muscle might be deficient in DMD patients and SMA patients.373 374 There is a risk of increased muscle injury when respiratory muscle training is applied. DMD’s current recommendations do not endorse the use of respiratory muscle training for this patient group. Please continue to study.326
Level of evidence 4
Research recommendations
- More research is needed to confirm that respiratory muscle training can be safe for patients suffering from Duchenne muscular dystrophy or spinal muscle atrophy.
More research is needed to confirm that respiratory muscle training can be safe for patients suffering from Duchenne muscular dystrophy or spinal muscle atrophy.
- More research is needed to establish if respiratory muscle training can be beneficial for patients suffering from other neuromuscular diseases.
More research is needed to establish if respiratory muscle training can be beneficial for patients suffering from other neuromuscular diseases.

Exercises for the Respiratory Muscle
Because of their heterogeneity, it is hard to synthesize the findings of these studies. There have been studies that have focused on adults, 363-366 other subjects only, 367-372 others which included both paediatric and adult subjects. Some also included people with various diseases and severity. Additionally the studies used different respiratory muscle training protocols–for example, duration of respiratory muscle training varied widely, from just 3-5 weeks364 to 2 years.372 Frequency ranged from once daily five times a week364 to four times daily.363 Outcome measures also varied between studies. In this study, there is not enough evidence to prove or disprove the effectiveness of any training program or respiratory muscle training in this patient population.
Paced breathing
Inhale and exhale according to the patient’s preference. It is thought to reduce dyspnoea during activity, for example when climbing the stairs or walking, and to help avoid rushing, breath-holding or rapid shallow breathing. It utilises a combination of the above techniques to suit the activity and the patient.
Evidence Level 4
Recommendation
- Teaching paced breathing is a technique to help patients suffering from COPD maintain their breathing control and decrease dyspnoea when exerting. (Grade D)
- Teaching paced breathing is a technique to help patients suffering from COPD maintain their breathing control and decrease dyspnoea when exerting. (Grade D)
Teaching paced breathing is a technique to help patients suffering from COPD maintain their breathing control and decrease dyspnoea when exerting. (Grade D)
Good practice point
- Combining techniques is a good idea.
- Combining techniques is a good idea.
Consider combining techniques.
Research recommendation
- Additional research is needed to determine the effectiveness and use of various breathing techniques.
- Additional research is needed to determine the effectiveness and use of various breathing techniques.
Additional research is needed to determine the effectiveness and use of various breathing techniques.

The Intermittent Positive Pressure Breathing in Acute Copd Exacerbation
Evidence Level 4
Recommendation
- Consider intermittent positive pressure breathing in acute exacerbations of COPD where patients present with retained secretions but are too weak or tired to generate an effective cough. (Grade D)
- Consider intermittent positive pressure breathing in acute exacerbations of COPD where patients present with retained secretions but are too weak or tired to generate an effective cough. (Grade D)
In acute COPD exacerbations, consider intermittent positive pressure breathing. Patients with COPD have retained secretions and are too tired or weak to produce a cough. (Grade D)
Good practice point
- Intermittent positive pressure breathing may be considered in acute exacerbations of COPD where patients do not have immediate access to non-invasive ventilation and intubation is not an option.
- In acute COPD exacerbations, intermittent positive pressure breathing might be an option. This is because patients don’t have access to noninvasive ventilation immediately and intubation may not be possible.
Intermittent positive pressure breathing may be considered in acute exacerbations of COPD where patients do not have immediate access to non-invasive ventilation and intubation is not an option.
Pelvic Floor Muscle Training
103 to 106
The main factor thought to influence this, chronic cough, is present in those with non-CF-related bronchiectasis in addition to risk factors common in the general population, for example following pregnancy. The majority of symptoms are not reported and people are less likely to seek treatment. An individual may experience urinary incontinence if they are unable or unwilling to do certain exercises.
Although there is no evidence in this population, intervention by a specialist continence physiotherapist in those with COPD and CF produced positive effects.107 Voluntary contraction of the pelvic floor muscles just before and throughout a cough or huff, known as “The Knack”, has been used successfully to reduce stress-related leakage of urine in a general population.108 It is reasonable to extrapolate these findings to the non-CF-related bronchiectasis population.
Evidence Level 4
Recommendations
- Patients should be questioned about their continence status. (Grade D)
It is important to ask patients about their current continence status. (Grade D)
- Patients with chronic cough should learn to contract their pelvic floor muscles (“The Knack”) before coughing and forced expiration. (Grade D)
Patients with chronic cough should learn to contract their pelvic floor muscles (“The Knack”) before coughing and forced expirations. (Grade D)
- Patients should seek out a specialist in continence physiotherapist if they suspect leakage. (Grade D)
Patients should seek out a specialist in continence physiotherapist if they suspect leakage. (Grade D)
Postural Drainage And Manual Techniques
Recommendations
- Individually assess the effect and acceptability of gravity-assisted positioning in patients with cystic fibrosis. (Grade B)
Individually assess the effect and acceptability of gravity-assisted positioning in patients with cystic fibrosis. (Grade B)
- Individually assess the effect and acceptability of modified gravity-assisted positioning in individual patients with cystic fibrosis. (Grade C)
Modified gravity-assisted positioning can be evaluated individually for the individual patient with cystic Fibrosis. (Grade C)
- If patients using independent techniques are unable to clear secretions effectively, chest wall vibration should be considered. (Grade C)
If patients using independent techniques are unable to clear secretions effectively, chest wall vibration should be considered. (Grade C)
Intermittent Positive Pressure Breathing In Stable Copd
Long-term daytime use of short periods of IPPB in stable COPD has been shown to be of no therapeutic value,81-84 and this method of application of IPPB does not reflect either physiotherapy clinical practice or current knowledge of effective use of NIV.
Level of evidence 1++
Recommendation
- Short periods of daytime intermittent positive pressure breathing should not be used to treat chronic respiratory failure in stable COPD. (Grade A)
- Short periods of daytime intermittent positive pressure breathing should not be used to treat chronic respiratory failure in stable COPD. (Grade A)
For chronic COPD patients with stable respiratory disease, short periods of intermittent positive pressure breathing during the day should be avoided. (Grade A)
Thoracic mobility and strength
Postural and musculoskeletal disorders are common among people with CF. There is a complicated relationship between respiration and posture.216-218
Thoracic kyphosis and vertebral wedging are more prevalent in people with CF than in healthy controls and are related to worsening lung function and clinical symptoms.216 218 There is also evidence of decreased thoracic mobility and muscle weakness compared with matched controls.218 These changes in soft tissue and spinal geometry are likely to be attributed to an increased work of breathing and the hunched posture assumed during excessive coughing. The major consequence is a high incidence of back pain, with severity associated with pulmonary deterioration, sputum production and breathlessness.216
Assessment and appropriate manual therapy treatment of posture correction, chest wall mobility and stretching exercises may decrease the pain and deformity, and prevent progression of these disorders.
Evidence Level 3
Recommendations
- Question patients with cystic fibrosis about musculoskeletal problems and back pain. (Grade D)
Ask patients suffering from cystic Fibrosis questions about back pain and musculoskeletal issues. (Grade D)
- If the problem is present, assess it and correct it. (Grade D)
Assess the problem if present and institute appropriate posture correction, chest wall mobility and stretching exercises or manual therapy treatments where indicated. (Grade D)
It’s a good point
- It is important to practice effective coughing and provide advice on how to position your body.
- It is important to practice effective coughing and provide advice on how to position your body.
Effective coughing with appropriate positioning advice should be advocated.
Recommendations for research
- Further research is needed to establish the effectiveness of postural correction and exercise in reducing thoracic pain and deformity.
- More research is required to determine if postural correction or exercise can reduce thoracic pain.
Further research is needed to establish the effectiveness of postural correction and exercise in reducing thoracic pain and deformity.
Research and Clinical Findings
- Detailed History
- Inspection
- Palpation
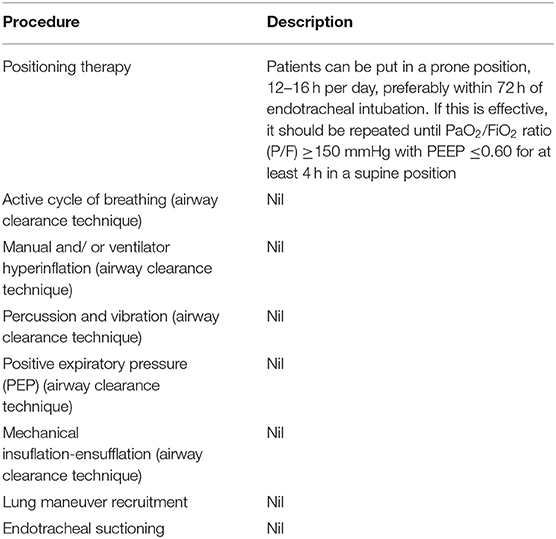
- Percussion
- Auscultation
- X-ray
When To Seek Help
Tahypnea and dyspnea should all be reported to your physician. Changes in the character of lung sounds, cough, and sputum production should also be reported. [10]
Take care
- bleeding from the lungs
- neck or head injuries
- Fractured ribs
- collapsed lungs
- damaged chest walls
- Tuberculosis
- Asthma severe
- recent heart attack
- Pulmonary embolism
- lung abscess
- active hemorrhage
- Some spine injuries
- recent surgery, open wounds, or burns
Manual Techniques
The physiotherapists use manual techniques such as chest wall percussion or thoracic compression with shaking or vibrations to improve airway clearance. They are most typically used in the UK in conjunction with the active cycle of breathing techniques; more commonly when the patient is unwell or fatigued and needing help with their usual regimen. Manual techniques are not as effective in clearing secretions than independent methods. There is little evidence.
Maintaining Training
One paper only has dealt with the maintenance of IMT73, concluding that IMT’s results would decline within one year if there was no maintenance program.
Level of evidence 2+
Recommendation
- Consideration of maintenance of an inspiratory muscle training programme is required. (Grade D)
- Consideration of maintenance of an inspiratory muscle training programme is required. (Grade D)
It is important to consider the maintenance of an inspiritory muscle-training program. (Grade D)

Exhalation
- The major function of the respiratory system is gas exchange.
- Cystic fibrosis
- Bronchiectasis
- Lung abscess
- Neuromuscular disorders
- Pneumonias in dependent lung regions.
- ICP Increased
- Unstable head or neck injury
- Hemodynamic instability, hemoptysis or active hemorhage can cause hemodynamic hemorhage
- Recent spinal injury or injury
- Empyma
- Bronchoplueral fistula
- Rib fracture
- Fail chest
Signs and Symptoms
These signs and symptoms are indicative of an ineffective airway clearance:
- Abnormal breath sounds (crackles, rhonchi, wheezes)
- Abnormal respiratory rate, rhythm, and depth
- Dyspnea
- Excessive secretions
- Hypoxemia/cyanosis
- Inability to remove airway secretions
- Ineffective or absent cough
- Orthopnea
On Your Sides
- With pillows under your hips, lie on one side so that your chest is lower than your hips.
- To clear congestion from the bottom part of the right lung, lie on your left side.
- To clear congestion from the bottom part of your left lung, lie on your right side.
The Nursing Care Plan for Ineffective Clearance of Airways 3
Foreign Body Obstruction
Nursing diagnosis: Improper airway clearance due to foreign bodies. This can be evidenced by anxiety and nasal flaring.
Desired Outcome: The patient will maintain a clear, open airway as evidenced by a normal breathing pattern.
Learning Outcome
- Define atelectasis
- Recognize the risk factors of atelectasis
- Comparing obstructive and non-obstructive dietsis
- Discuss the expected diagnosis and assessment of atelectasis patients
- Choose the appropriate nursing intervention to help a patient suffering from atelectasis.
- Define medical procedures that can be used to treat atelectasis
- Identify key patient education interventions
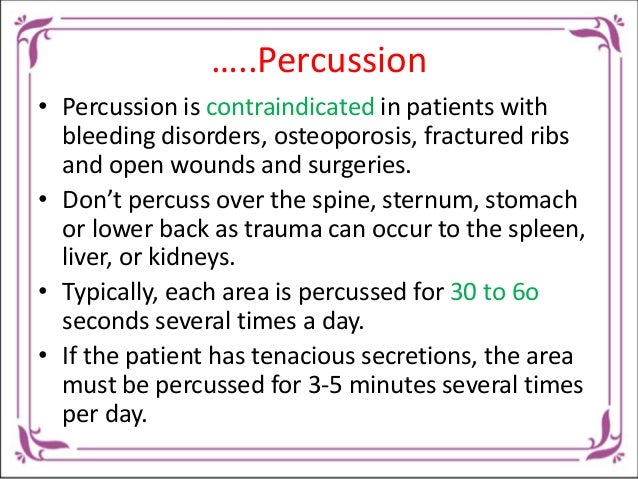
Chest Physiotherapy Nursing Interventions
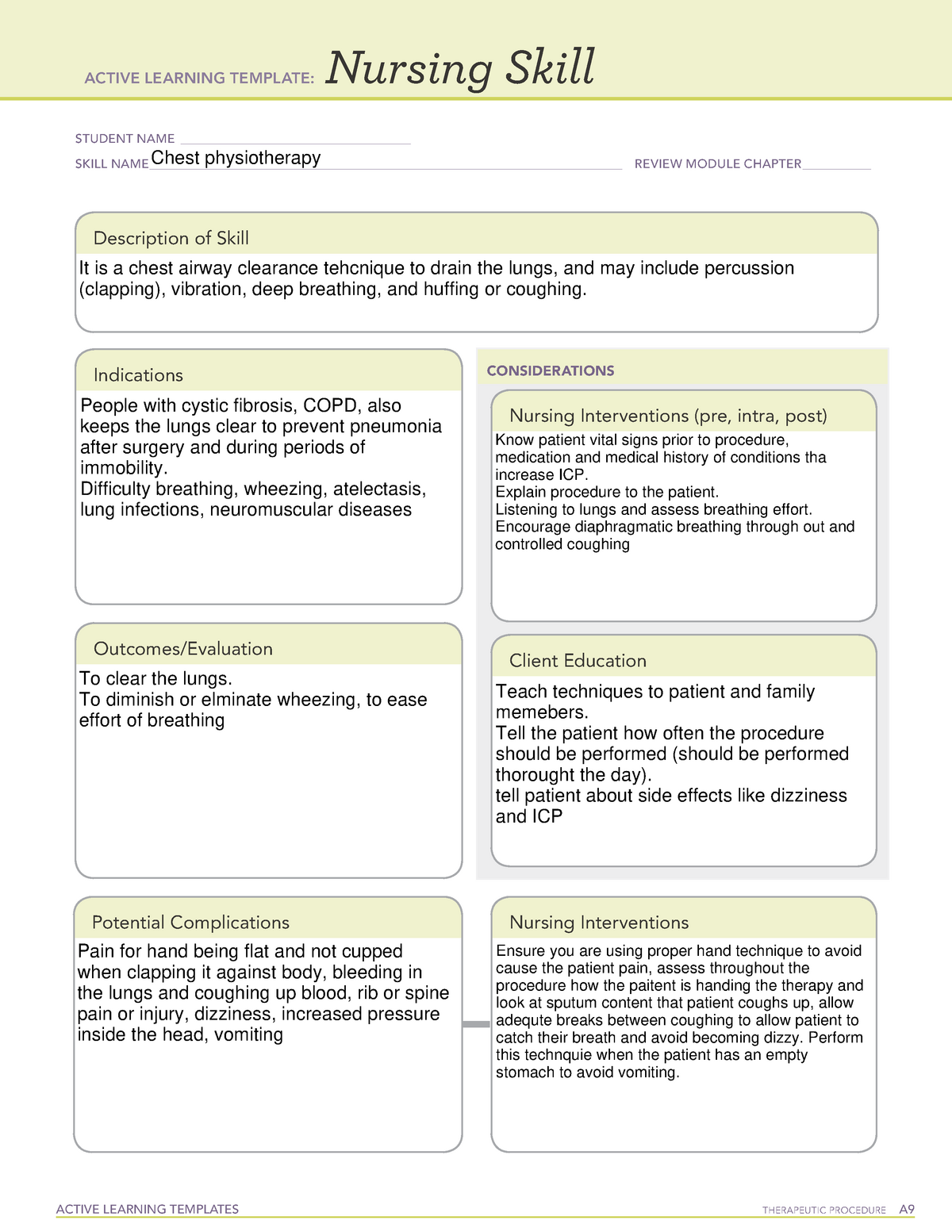
Therapeutic Procedure
STUDENT IDENTIFICATION _____ PROCEDURE NAME____ REVIEW MODULE CHAPTER___ ACTIVE LEARNING MODEL:
Description of Procedure. Indications. Results. Evaluation CONSIDERATIONS. Nurse Interventions. (pre, intra., post) Client Education. Weston Hilland Chest Physiotherapy. 53. This procedure removes the secretions from our lungs.
Clients who are suffering from thick secretions or difficulty clearing their airways should consider this type of therapy.
Use Postural drainage for increased movement secretion, broken down by vibrations or percussion.
Before you begin, explain the process to your client. Also tell them why it is used. Inform the client about the Huffing technique.
Pre: Check for contraindications. Use a cup-hand method to percussion the posterior chest wall. Post: Position the client in order to aid with postural drainage, based on their affected lung regions.
Diarrhea, Vomiting, Dizziness, Damage to Ribs, Pain Pulmonary Hemorrhage and Bronchospasm.
Results: Client is now able expectorate sputum, and can clear their airways. Evaluation: The client reports less shortness of breath and showcases better SPO2 levels.
Abstract
Objective: To determine associations between respiratory nursing diagnoses and nursing interventions in patients submitted to thoracic or upper abdominal surgery.
Method: Cross sectional quantitative study. Within the first 48 hours following thoracic, or upper abdominal surgery, 312 patients were included. Patients were examined by the research team using an instrument with variables related to the respiratory function. Three nursing diagnoses were identified by the research team. The researchers then proposed treatments using the NANDA-I Classification, as well as the Nursing Interventions Classification. The chi-square and Fisher’s tests were used to test correlations.
Out of 312 examined patients, ineffective or inefficient airway clearance was identified in 185 (59.3%), 123 (39.4%), 141 (45.4%) and 141 (1,8.4%). It was found that patients suffering from ineffective airway clearing were more likely need to have pain management (or 2.27), chest physical therapy (or 2.96), or positioning (or.1.8) whereas patients experiencing impaired gas exchange (or 0.28), were less likely to need to manage their airway (or 0.13), or to receive chest physiotherapy.
Conclusions: Ineffective airway clearance was associated with more patients needing pain management, chest therapy, positioning and chest physiotherapy. Nursing diagnosis of impaired gas exchange related to airway management and chest-physiotherapy. This information provides nurses with the basis to create effective care plans, and minimize any postoperative complications.
Keywords: Atencion de enfermeria; Diagnostico de enfermeria; Enfermeria postanestesica; Nursing care; Nursing diagnosis; Patient care planning; Planificacion de atencion al paciente; Postanesthesia nursing.
Copyright (c) 2019 Elsevier Espana, S.L.U. All rights reserved.

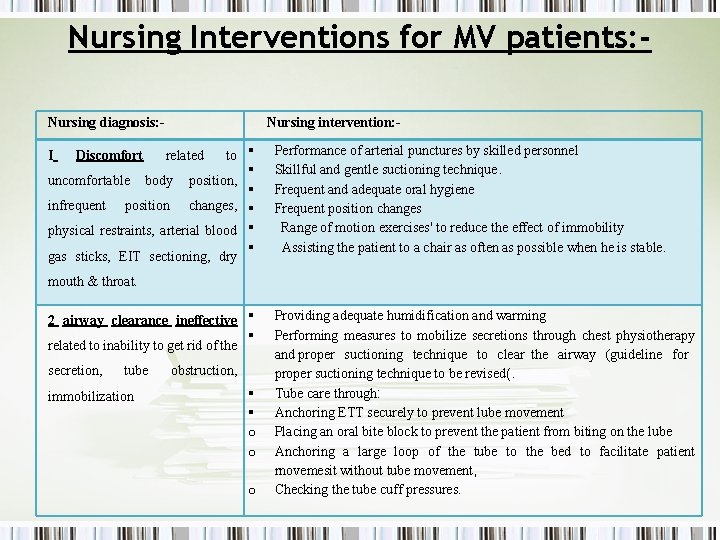
Abstract
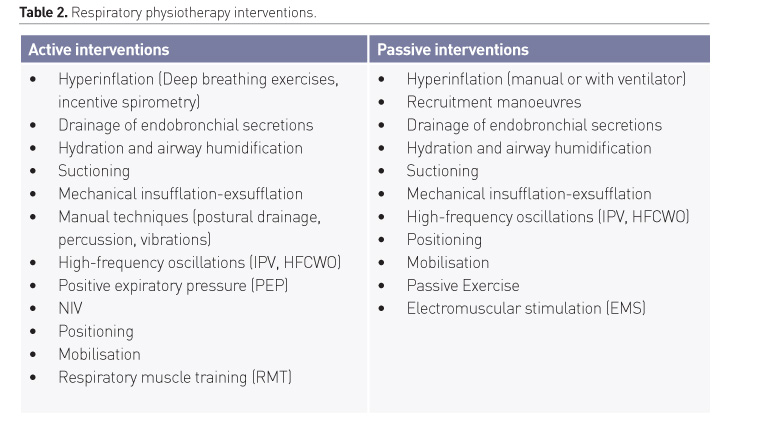
Long periods of inactivity and bed rest can have adverse effects for patients admitted to intensive care units. A common condition many patients face during stays in intensive care units is breathing difficulty. Our goal was to determine and assess the evidence to recommend nonpharmacological or technical interventions to combat breathing difficulties. This is a PRISMA-compliant report. Systematic searches were conducted in MEDLINE EMBASE, Cochrane, and EMBASE. An O’Malley and Arksey framework was used for a scoping analysis. All in all, 1190 records were found. 27 were also included in the review. Chest physiotherapy, chest exercises, breathing techniques and inspiratory muscles training were some of the interventions that targeted breathing problems. Several of the interventions showed minor beneficial effects. However, because of limitations in the studies, the findings are inconclusive and need further research.
critical ill patient nursing respiration scoping overview Access Options
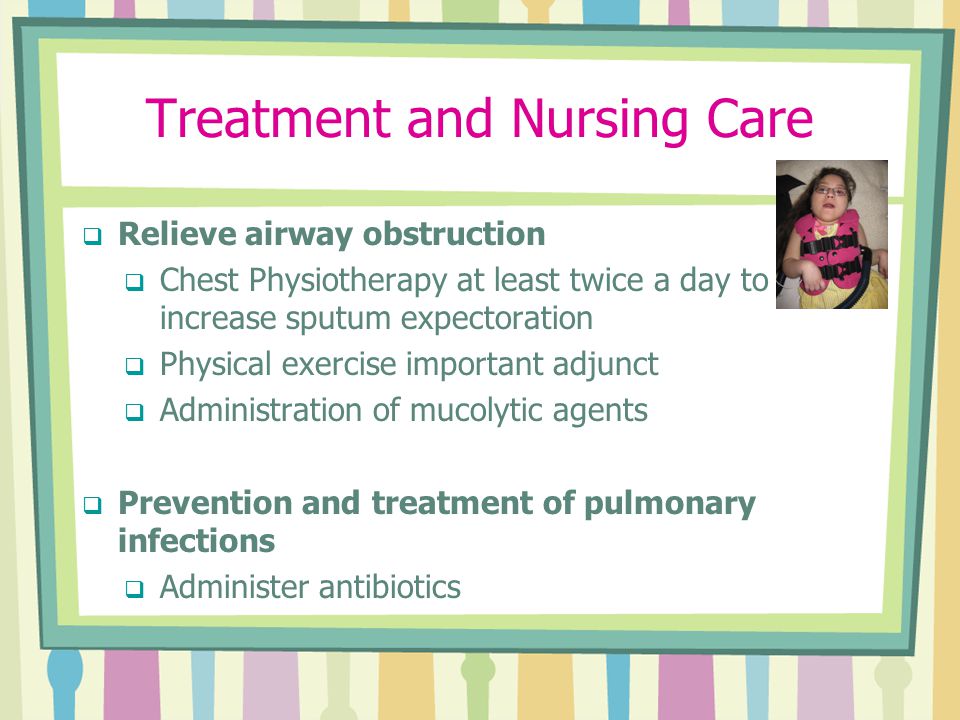
What are the Nursing Interventions for Chest Physiotherapy?
External mechanical maneuvers are used in chest physiotherapy to increase mobilization and clear airway secretions. They include postural drainage and vibration.
These are 3 methods used to perform chest physiotherapy.
Chest physical therapy or CPT (or Chest PT) refers to an airway clearance procedure (ACT) that involves draining the lungs. This may include percussion (clapping), vibration, deep breath, huffing or coughing.
Do Nurses Do Chest Physiotherapy?
Traditional chest physiotherapy may still be used by nursing professionals to treat critically ill patients.
What should I do before chest physiotherapy?
Chest physiotherapy is a process that can help you feel more comfortable and have a better outcome. You should not eat right before chest PT. In order to reduce the thickness of your lungs, you may be asked to consume water.
.Chest Physiotherapy Nursing Interventions
Kent Chiro-Med Wellness Clinic
| Website | https://www.kentchiromed.com/ |
| Address | 563 Gladstone Ave, Ottawa, ON K1R 5P2, Canada |
| Phone | +1 613-508-0113 |
| Category | Physiotherapy Ottawa |
Beverly Physiotherapy
| Website | http://www.beverlyphysiotherapy.com/ |
| Address | 747 Ellice Ave, Winnipeg, MB R3G 0B5, Canada |
| Phone | +1 204-774-8385 |
| Category | Physiotherapy Winnipeg |




















:fill(white)

