Chest Physiotherapy Devices

Abstract
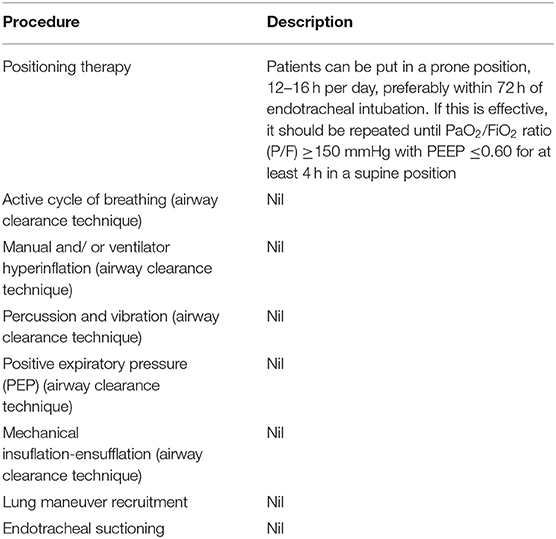
Recent years have seen a wide range of devices used by patients with severe respiratory problems. They help to remove mucus from the lungs and enhance pulmonary function. As a result of a literature review, this research aims to examine the effectiveness current devices in respiratory physiotherapy. Current devices for physiotherapy in patients with severe respiratory conditions are described as an alternative or supplemental treatment and can encourage patients to do their therapy themselves. They are easy to use, independent of treatment and can increase patient compliance. These devices are the Positive Expiratory Pressure, the High Frequency Chest Wall Oscillation, the Oral High Frequency Oscillation, the Intrapulmonary Percussive Ventilation, the Incentive Spirometry the Flutter and the Acapella and the Cornet. Studies have demonstrated that the effectiveness of current devices is in terms mucus expectoration, pulmonary function improvement and custodial care. To ensure patient compliance, the physiotherapist has to choose the best device. Because of the limited number of studies published, it is necessary to conduct more controlled trials.
Politique
Aetna views home chest physiotherapy as medically required upon initial prescribing of chest physiotherapy. This is to stabilise the patient, and also to teach family members or caregivers how to provide chest physiotherapy. If the member has a weakened pulmonary condition, chest physiotherapy is medically required. A respiratory therapist cannot perform chest physiotherapy on a person whose condition is stable. However, a caregiver or family member can administer the treatment at home.
Cystic Fibrosis (CF), Chronic Bronchitis, Bronchiectasis and Immotile Cila Syndrome (also called primary ciliary dyskinesia and asthma) can be treated with airway oscillating devices, such as Flutter or Acapella.
For CF, immotile cilia, bronchiectasis and chronic bronchitis (e.g. Fluid Flo, Frequencer and VibraLung Acoustical percussor), mechanical percussors are medically required.
A positive expiratory pressure mask (PEP) is medically required for CF and immotile cilia Syndrome, CF, and Chronic Bronchitis.

Background
Cystic fibrosis (CF), chronic bronchitis/bronchiectasis/immotile cilia syndrome, asthma and other acute respiratory tract infections may cause an abnormal airway clearing or increase in sputum. In addition to mucociliary clearing (MCC), other mechanisms, such as cough and peristalsis or two-phase liquid-gas flow, alveolar clearance, and peristalsis are used for the elimination of airway secretions. Each illness has a different underlying cause. CPT stands for chest physiotherapy. This is a treatment that aims to improve abnormal airway drainage. It decreases obstruction in the airways and their consequences such as hyperinflation and atelectasis. Furthermore, by removing infected mucopurulent secretsions, physiotherapy may decrease proteolytic tissue destruction. The decline in lung function is slowed by methods to increase the removal of tenacious lungs secretions.
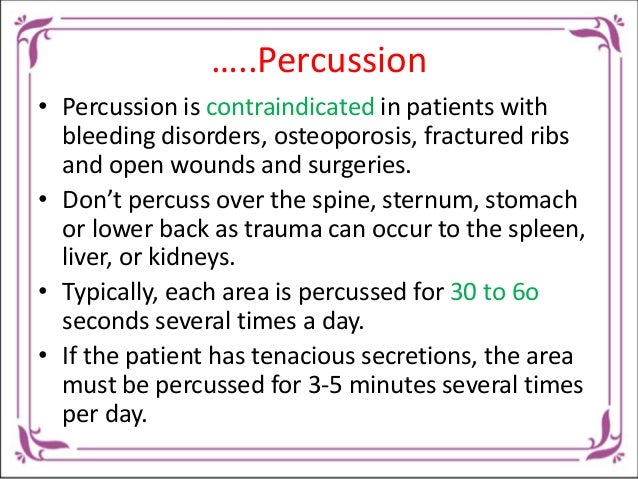
The most commonly used method for pulmonary care is still clapping and vibration. Most practitioners prescribe 20 to 30-min CPT sessions 1 to 3 times a day, depending on the severity of disease and the presence of intercurrent infection.
Family members and other caregivers may be trained to administer CPT, or help with the administration of manual CPT for children. According to the National Heart Lung and Blood Institute (1996) of the National Institutes of Health, “Chest therapy is bronchial or postural drainage. This involves placing the patient in an area that permits drainage of mucus from their lungs. The mucus is also moved out of the airways by vibrating the back or chest (percussed). Repeat this procedure on various parts of the back and chest in order to loosen different types of mucus. For children, this procedure must be performed by their family. However, older patients may learn how to perform it themselves. You can buy mechanical equipment that helps with chest physical therapy. Different kinds of airway clearance equipment have been designed for self-use and require very little to no assistance from others. Alternative methods can be used if a qualified caregiver is unable to manually administer CPT. These techniques were developed using CF patients.
De Boeck and others (2008) observed that children living with CF and bronchiectasis should use airway clearance methods. These techniques are sometimes prescribed for children in good health with an acute breathing problem. The investigators looked at the evidence supporting this type of treatment in children with no underlying diseases. They stated that few studies have been performed; many different techniques are available and the therapies used are often poorly specified. Name the airway clearance method used for treatment. It’s better to say “chestphysiotherapy” than just saying “chest clapping,” which can be confusing with vibration plus postural drainage or chest clapping. Evidence is lacking that airway management techniques can be used to manage children with acute breathing problems. Physicians routinely prescribing airway clearance techniques in previously healthy children should question their practice.
Systems for high frequency chest compression
A high-frequency compression device for the chest (formerly The Vest Airway Clearance System) (Advanced Respiratory St. Paul MN) is an inflatable vest attached to a compressor. This provides external high frequency chest wall oscillation. A tubing connects the vest to an air pulse delivery device. To inflate the vest and release it against the chest, the patient presses a foot pedal.
Patients with CF have reported increased sputum production by high-frequency chest compression devices. A abnormality in chloride-ion transport at the apical epithelial cell surface is responsible for cystic fibrosis. Increased viscosity can be caused by the altered composition of secretions from epithelial surfaces affected. High-frequency chest compression devices may be particularly useful in clearing abnormal secretions. This is because vibrational shear forces, which facilitate expectoration and reduce the viscosity in these secretions, can aid in expectoration. It’s similar to shaking jello that causes it become fluid. But, chest compression vests that use high frequency frequencies have not shown to be any more effective than manual chest physical therapy. For patients who are unable to receive manual chest physiotherapy, it can be substituted.
The use of high-frequency compression devices for chest wall problems other than CF has been encouraged, even if the condition is not CF bronchiectasis. However, there are no adequate published controlled clinical studies of high-frequency chest compression devices for conditions other than CF. Due to the unusual pathophysiology of CF which causes a abnormal production of CF serum, it is impossible for evidence of effectiveness of high frequency chest wall compression devices in CF to be applied to other pulmonary diseases. FDA approved Vest for many conditions including pulmonary.
A lack of adequate research has also prevented high frequency chest compression from being compared to simpler and less costly devices, such as Flutter or Acapella, that use high-frequency oscillations on the airways.
American College of Chest Physicians’ non-pharmacologic, evidence-based clinical practice guidelines for airway clearing therapies (McCool & Rosen 2006) suggest that oscillatory devices (e.g. Flutter and IPV) should not be used in place of chest physiotherapy.
Only the Vest can be purchased. The air pulse delivery system, an air-pulse generator and flexible hoses may also be available for rent or purchase.
It is not clear whether high-frequency chest physiotherapy equipment should be used for any indications other that CF.
Yuan and others (2010) have stated that in cerebral palsy (CP), as well as neuromuscular diseases, airway infections and secretions can be common. Chest physiotherapy is standard therapy but effort is substantial. The use of high-frequency, chest wall oscillations (HFCWO), in CF is limited. Safety data and tolerability in cerebral palsy are also not known. Researchers conducted a prospective, randomized and controlled study of HFCWO and standard CP in patients with neuromuscular disorder or CP. Outcome measures included respiratory-related hospitalizations, antibiotic therapy, chest radiographs, and polysomnography. Concerning therapy compliance, caregivers were asked questions. Total 28 people enrolled. 23 had completed (12 CPT), the mean duration of the study was 5 months. We have not heard of any adverse outcomes. HFCWO was associated with higher compliance to the prescribed regimen (p = 0.036). These findings indicate safety, ease of use, and greater compliance with HFCWO. A better airway clearance might help reduce hospitalizations. To confirm the results, larger controlled trials will be needed.
Drosman and Jones (2005) noted that, in the pediatric population, HFCWO is most widely used in children with CF, but that children with developmental disorders involving neuromuscular dysfunction also have impaired airway clearance with or without ventilatory dependence. According to the authors, “[l]arge and long-term studies of HFCC in patients with developmental disorders are required.” Lange et.al. (2006) measured changes in respiratory function following HFCWO in patients with amyotrophic lateral sclerosis. The 12-week-long study involved HFCWO treatment in patients suffering from probable or definite ALS. It included a Amyotrophic Lateral Sclergy Functional Rating Scale respiratory subscale score of 11 or greater, and forced vital capacity (FVC), greater or equal 40 %. There were 46 participants (21 men and 25 women, 58.0+/- 9.8 years), 22 of whom received HFCWO treatment while 24 others were left untreated. Only 35 completed the trial: 19 used HFCWO and 16 untreated. Data were reported per protocol and not according to intention-to–treat. HFCWO patients had less coughing at night and breathlessness at 12 weeks (p 0.021), compared to baseline. HFCWO customers reported less breathlessness (12 weeks), while non-users had more difficulty breathing (p 0.027). FVC change and peak expiratory flow, oxygen saturation, fatigue or functional quality of living index were not significantly different. FVC was measured in patients who had FVC between 40 % and 70 %. However, FVC levels were significantly lower in patients not treated with HFCWO. Patients suffering from HFCWO suffered less fatigue and increased breathlessness. Satisfaction with HFCWO was 79 %. The authors concluded that HFCWO was well-tolerated, considered helpful by a majority of patients, and decreased symptoms of breathlessness. HFCWO showed an increase in fatigue among patients who had impaired breathing and a tendency to slow down the decline in forced vital capacity. Although the researchers explained that HFCWO was exploratory in design, it could not have detected significant differences in clinical outcomes.
Chaisson et al (2006) didn’t find HFCWO of any significant benefit to patients living with ALS. The effectiveness of HFCWO given through the Vest Airway Clearance System was evaluated in conjunction with standard care to prevent pulmonary complications in patients suffering from ALS and prolong the time until death. A total of 9 patients with a diagnosis of ALS and concurrently receiving non-invasive ventilatory support with bi-level positive airway pressure (BiPAP) were recruited from an outpatient clinic. Patients were randomly allocated to either standard or enhanced care. 5 patients also received HFCWO for an additional 15-min-long period. From the moment of death to longitudinal evaluations of oxyhemoglobin saturation and forced FVC as well as adverse events, were performed. Through the entire study, pulmonary complications such as pneumonia, atelectasis and hospitalization for an abnormality in the respiratory system, as well as tracheostomy (with mechanical ventilation) were closely monitored. FVC declined at a similar rate in all treatment groups. There was no difference between them. HFCWO HFCWO Airway Clearance did not increase the time till death, compared to standard therapy (340 Days +/-247 versus 470 Days +/- 241); p = 0.26 Patients with ALS who are concurrently receiving BiPAP did not experience any clinical benefit in terms of either mortality or loss of lung function. HFCWO could be of benefit to patients suffering from ALS with co-existent pulmonary disease, pre-existing mucus related pulmonary complications, and less severe respiratory muscle weakness.
Positive expiratory pressure (Pep).
This valve increases the resistance of expiratory airflow in the mask/mouthpiece. Inhaling and exhaling, the patient inhales 5-20 times. Monitor the pressure and adjust it with a manometer. There are two options: low pressures, or high. This mask/mouthpiece, called the PEP Mask/mouthpiece, achieves similar results to autogenic drainage.
Studies on the efficacy of PEP were mostly conducted in Europe. These studies showed that PEP was comparable to other techniques for airway clearance. The results of the published reviews showed that PEP was comparable to other techniques (postural drainage forced expiratory technique) in clearing sputum. The strongest evidence of the effectiveness of PEP comes from a 1-year randomized controlled clinical trial of PEP versus conventional physiotherapy in 40 children with CF. PEP treatment led to improvements in lung function in the patients, while conventional physiotherapy caused a decline in this area. For changes in FVC or FEV1, statistically significant differences were observed between the treatment groups.
There are numerous PEP Mask/PEP Valves on the market. Here are some examples: Resistex PEP Mask, Mercury Medical, Clearwater, FL, TheraPep Valve, DHD Healthcare, Inc., Canastota, NY), Acapella, DHD Healthcare, Inc., Wampsville, NY, PARI PEP Mask, PARI Respiratory Equipment, Inc., Midlothian, VA.
The Intrapulmonary Percussive Valve (IPV), an aerosol machine, delivers pressurized gas minibursts at a rate of 100-225 cycles/min into the respiratory tract. Under pressure, aerosolized drugs can be given with oscillations which vibrate the chest. IPV permits continuous, monitored positive pressure applications and percussion through the whole respiratory cycle. You can control factors such as the inspiratory period, peak pressure and delivery rate. The Percussionaire has 510(k) status with the FDA.
Unfortunately, there is not enough scientific data available to prove the efficacy of IPV. Homnick et.al (1995), found that IPV preserved lung function in the same way as traditional aerosol or chest physiotherapy. Newhouse et. al. (1998) found that IPV is more effective than standard chest physiotherapy in preserving lung function. They also needed longer and larger studies to determine its utility for the independent administration of chest physiotherapy. There are not any studies that show IPV is better than pulmonary care at the hospital. Also, there have been no home-based studies.
Reychler et. al. (2006) state that IPV (often combined with an nebulizer) is more commonly used as a form of physiotherapy. But, it is not clear if the IPV’s physiological or clinical benefits have been studied. These researchers compared lung deposition of amikacin by the nebulizer of the IPV device and that of standard jet nebulization (SJN). Amikacin were nebulized by both devices on a group consisting of 5 healthy people during spontaneous breathing. Urograin monitoring measured the amikacin’s deposition. Drug output of both devices was measured. Respiratory frequency (RF) was significantly lower when comparing the IPV device with SJN (8.2 +/- 1.6 breaths/min versus 12.6 +/- 2.5 breaths/min, p < 0.05). With IPV, the total amount of amikacin in urine per day was lower than that with SJN (0.8% versus 5.6% initial doses; p = 0.001). Each device had the identical half-life for elimination. IPV output was less than SJN. The amount of amikacin delivered to the lung is 6-fold lower with IPV than with SJN, although a lower RF was adopted by the subjects with the IPV. These authors conclude that IPV may not be favorable to the nebulization for antibiotics.
Bruckner (2008) reported that patients with neuromuscular conditions (NMDs) have weaker coughs and can use mechanical aids such as assisted coughing. Breathing techniques, as well as special devices like Flutter and Acapella can be used in cases of preserved respiratory muscles to stimulate secretion during airway infections. These physiotherapeutic approaches were summarized as oscillating physiotherapy. Their mechanisms are dependent on separation of the mucus from the bronchial wall by vibration, thus facilitating mucus transport from the peripheral to the central airways. They are well-established for mucoviscidosis or chronic obstructive. But, it is not clear if they can be used in NMD. Simple oscillating therapies require a strong respiratory muscle force to be effective. The Percussionaire, i.e., IPV or high-frequency chest walls oscillation (HFCWO) are exceptions. These approaches can cause weaker patients to become exhausted or over-strained in daily clinical practice. A general recommendation for the adoption of simple oscillating physiotherapeutic interventions can not be made in patients with NMD. Perhaps HFCWO, or IPV, will become more useful in NMD patients.
Percussionaire Corp Sandpoint ID has developed the Impulsator F00012, an intrapulmonary percussive ventilation device. It is a pneumatic device which delivers high-flow rate bursts and aerosols to the lungs at speeds of between 200 and 300 cycles per minute. At a maximum pressure of 20 to 40% H2O, pulse breaths can be delivered. The pressure is titrated through visualizing the percussive movement within intercostal spaces. A mouthpiece delivers breaths and then the lungs are stimulated for 5 to 15 seconds over a 30-minute period. Evidence is lacking regarding the effectiveness and safety of Impulsator F00012.
Kallet (2013) stated, “Many patients in respiratory distress who are on mechanical ventilation have special requirements. They may need inhaled therapy to reduce airway obstruction or treat pulmonary disease, improve their pulmonary hygiene, or to stabilize the gas exchange. These therapies tend to be supportive, not curative. Most of the evidence currently supporting routine use is lacking. In this overview, the author described the rationale and examined the evidence supporting adjunctive therapies during mechanical ventilation. Mechanistic as well as clinical research indicate that IPV could increase lung secretion mobilization, and possibly reverse atelectasis. However, its impact on outcomes such as ICU stay is uncertain. The most crucial issue is whether aerosolized antibiotics should be used to treat ventilator-associated pneumonia, particularly when caused by multi-drug resistant pathogens. Numerous studies provide encouraging evidence supporting the use of aerosolized antibiotics, at least when used in specific cases. Inhaled lung vasodilators can provide some short-term oxygenation improvement and could also be used to stabilize pulmonary gas exchange in complicated management scenarios. Uncontrolled, small studies indicate that patients who have suffered severe inhalation injury may experience pulmonary castings breaking down and airway obstruction. Similar low-level evidence suggests that heliox is effective in reducing airway pressure and improving ventilation in various forms of lower airway obstruction. These therapies are usually supportive and could help patients manage their conditions. However, because they have not been shown to improve patient outcomes, it behooves clinicians to use these therapies parsimoniously and to monitor their effectiveness carefully.
Branson (2013) said that postoperative complications of the lungs (PPCs), are frequent and costly. Costs, morbidity, and mortality are higher with PPCs than with cardiac or thromboembolic complications. PPCs can be prevented and treated by respiratory therapists using various techniques including continuous positive pressure, incentive-spirometry, and chest physical therapy. This is despite the lack of scientific evidence.
What are the 3 Types Of Chest-Physiotherapy?
A chest therapy session includes chest percussion and postural drainage. It also involves turning, deep breathing exercises and coughing. Some of the most recent devices for chest physical therapy, including the positive expiratory pressure valve (PEP), and the flutter, were introduced in the 2000s.
What are the Essential Techniques for Chest Pain Physiotherapy?
Chest physical therapy or CPT (or Chest PT), is an ACT to remove the lungs. The technique may use percussion, vibration, deep breath, huffing or coughing.
What is the Part of Chest Physical Therapy?
These devices include the Positive Expiratory pressure, the High Frequency Cest Wall Oscillation (HFCO), the Oral High Frequency Oscillation (OHFO), the Intrapulmonary Percussive Vailation, and the Incentive Spirometry, as well as the Acapella, Cornet, and the Flutter.
Which Technique Is The Most Effective For Chest Physiotherapy?
The routine of chest physiotherapy is twice daily. It may be increased in frequency during severe bronchitis episodes. Postural drainage and percussion are the most popular methods.
.Chest Physiotherapy Devices
Kent Chiro-Med Wellness Clinic
| Website | https://www.kentchiromed.com/ |
| Address | 563 Gladstone Ave, Ottawa, ON K1R 5P2, Canada |
| Phone | +1 613-508-0113 |
| Category | Physiotherapy Ottawa |
Beverly Physiotherapy
| Website | http://www.beverlyphysiotherapy.com/ |
| Address | 747 Ellice Ave, Winnipeg, MB R3G 0B5, Canada |
| Phone | +1 204-774-8385 |
| Category | Physiotherapy Winnipeg |























:fill(white)