Chest Physiotherapy Cpt
Vs. Vest therapy – Manual Cpt
While manual CPT (or chest physiotherapy) using an Airway Clearance Vest are effective means of mobilizing mucus in both cases, there are significant differences.
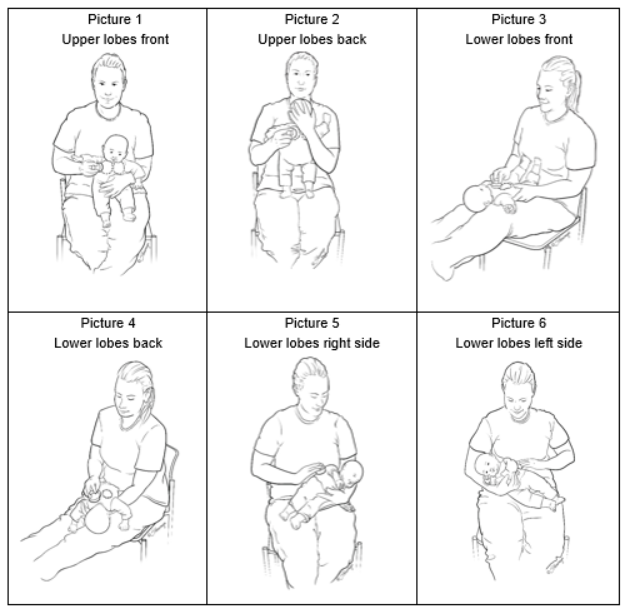
The main difference between >percussion vest therapy and manual CPT is that the former can be done independently. Manual CPT involves using gravity to expel mucus. A caregiver or therapist assists. For the removal of mucus, the caregiver may then move the patient toward the larger airways by percussion.
You can perform airway clearance therapy independently. It is best to do it right away, usually before you go to sleep. Each therapy session can be administered by the patient using a SmartVest Airway Clearance System, which uses a high-frequency chest wall oscillation therapy vest (HFCWO). SmartVest delivers rapidly repeating pulses of air that gently squeeze and release the upper body to help propel mucus toward the larger airways.1 how HFCWO therapy using the SmartVest works to clear mucus and manage bronchiectasis symptoms .
Abstract
Objective: Compare intrapulmonary percussive ventilation (IPV) to conventional chest physiotherapy (CPT) and determine their effects on improving atelectasis and static compliance in pediatric patients.
Methods. We performed a retrospective analysis of 46 patients who had received IPV therapy. The Percussionator IPV-1 ventilator operated at frequency frequencies of 180-220 cycles/min. Patients were given medicated aerosol treatment with albuterol 2.5 mg mixed in 6mL normal solution. The pediatric radiologist assessed the radiographs of both baseline and follow-up chests. An ordinal scoring system was used to assess the severity of atelectasis in chest radiographs. 4 = Complete collapse and 0 = Complete resolution. To compare static compliance with atelectasis, we did a prospective controlled, randomized study on intubated and mechanically ventilated subjects. Baseline and daily chest radiographs were evaluated using the same scoring system as in the retrospective pilot evaluation. Patients were ventilated using volume-controlled, synchroized intermittent mandatory ventilation. The tidal volume was 6-10 mL/kg. Patients were randomized to CPT (clapping and vibration) or IPV at frequencies of 180-220 cycles/min and pressures of 15-30 cm H(2)O (equal to the peak pressures on the ventilator), with 6 mL of normal saline solution via medicated aerosol. They were administered every 4 to 5 hours for approximately 10-15 minutes. Static compliance measurements were calculated from exhaled tidal volumes and plateau pressures.
Results: In the retrospective study the median age of patients receiving IPV was 4.2 years and the median duration of IPV was 6.2 days. A change in atelectasis score from 3 to 1 (p < 0.001) was seen. Patients were surveyed in a controlled, randomized trial. The average age was 3.1. Before treatment, atelectasis scores were similar between CPT and IPV (median 2.0 in each group, p=0.530). The CPT group's atelectasis score was unchanged (median 2.0 p=0.421), while the IPV group had a better average (median1.0 p=0.026). Average treatment duration was 6.2 and 2.1 days respectively in the CPT and IPV groups (p = 0.018). Treatment did not result in any changes in static compliance.
Patients who were treated with IPV therapy showed a significant clinical improvement in their atelectasis. Patients who received IPV therapy showed a clinically more significant increase in their atelectasis score than those receiving CPT. IPV, a method that allows patients to use artificial airways for alternative clearance of their airways, is safe and efficient.

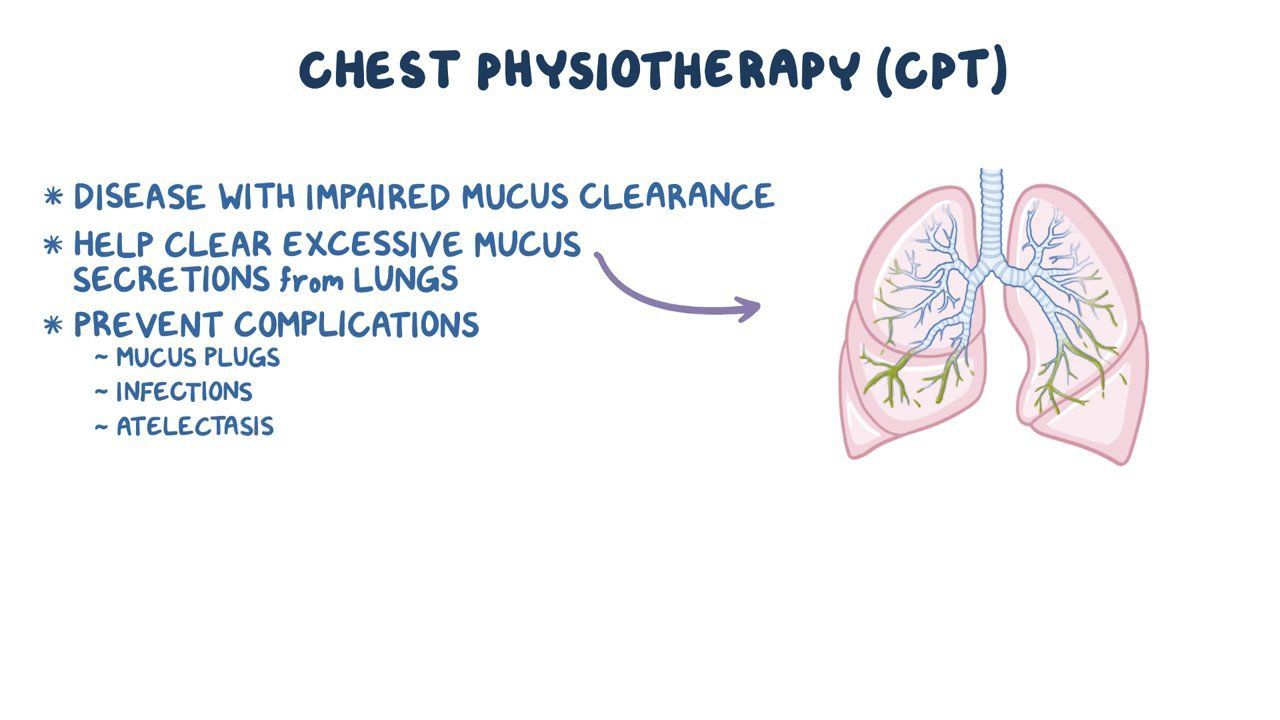
Chest Physiotherapy
Chest Specialty Respiratory Therapist Edit on Wikidata
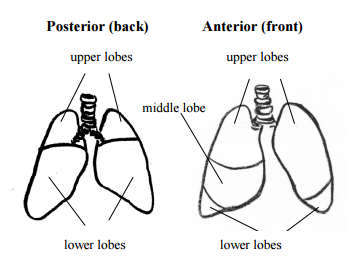
CPT is the treatment of chest that can be performed by respiratory therapists. It involves the indirect removal or enlargement of mucus passages. Others terms include cardio-thoracic or respiratory physiotherapy.
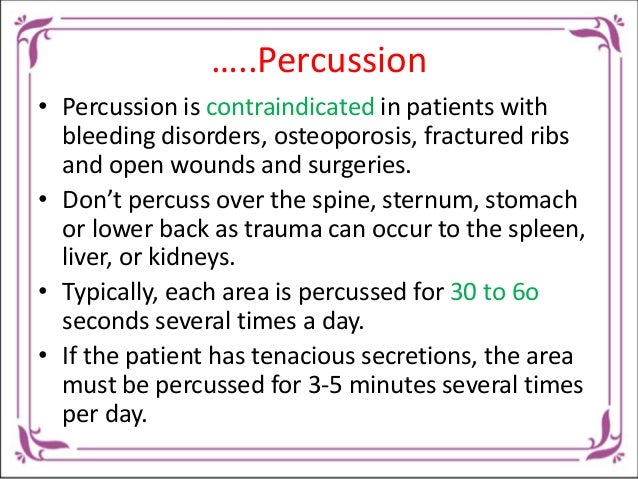
CPT is a treatment that’s used to treat mucus dysfunction. All of these conditions require chest physiotherapy in order to clear mucus. The therapist lightly taps the chest and underarms. While percussion is useful in treating infants and children it has been discontinued in adult treatment. It can be used to help with self-management and other issues. These include oscillating positive expiratory pressure devices or OPEP devices like the use of “Flutter”, “Aerobika”, “AirPhysio”, “Pari O-PEP” or Positive Expiratory Pressure PEP devices like the “Acapella” and PEP masks or devices ( positive expiratory pressure ) as well as specific exercise regimes. The exercises prescribed can include specific respiratory exercises e.g. Chest physiotherapy is considered to be a general treatment of adults suffering from pneumonia. It can include specific exercises such as breathing, autogenic drainage, or cardiovascular exercises to help the body remove sputum, improve oxygen efficiency, and reduce the risk of complications and physician involvement. Particularly, to improve the ventilation of areas with local lung obstruction. The goal of chest physiotherapy is to increase local lung expansion and increase perfusion. Airway obstruction and resistance should drop if secretions can be cleared from the larger airways. To increase lung compliance, it is important to reduce secretions and allow for better ventilation. If clearance of secretions from both large and small airways occurs, it is reasonable to assume that the work of breathing and oxygen consumption should decrease, and gas exchange improves. Additionally, these targets will help to reduce the risk of chronic and acute lung diseases such as postoperative respiratory infections and morbidity.
See also: Intrapulmonary pressure ventilator Postural drainage
What is Chest Physiotherapy and How Does It Work?
Chest physiotherapy is a group of physical techniques that improve lung function and help you breathe better. CPT, which is chest physiotherapy or CPT, expands the lung, strengthens breathing muscles, reduces thick lung secretions, and allows for better drainage. Chest PT helps treat such diseases as cystic fibrosis and COPD (chronic obstructive pulmonary disease). It helps to keep the lungs healthy after surgery as well as during immobilization.
Only one treatment method for respiratory disease is chest physiotherapy. You should get another opinion on all your options before you consider chest physiotherapy.
To help reduce lung secretions, chest percussion is used. Some patients wear a special CPT vest hooked up to a machine. In order to dissolve the secretions in the body, the machine causes the vest vibration at high speed.
You can use controlled coughing to break down your lungs. Your caregiver will either suction them or you can blow them out.
Deep breathing to improve the function of your lungs. You may use it after surgery to re-expand your lungs and prevent pneumonia.
Positioning and turning from side to side to help improve lung expansion and drainage of secretions. This is important for patients who are bedridden or hospitalized.
Postural drainage to help drain lung secretions Other procedures that may be performed Doctors generally recommend one or more other treatments to manage respiratory disease and breathing problems. Treatments will vary depending upon the type and severity of your condition, as well as your medical history, age, and other factors. The following procedures and treatments for chest PT may be available:
What is the Best Thing to Do After a Chest Physiotherapy Treatment?
It is difficult work to do chest PT. However, your ability to tolerate the therapy more will increase as you improve. Your provider should be notified if you’re feeling tired or unwell so they can adjust the methods. Over time, chest physiotherapy can help you breathe easier, increase the amount of oxygen in your blood, and improve your energy level.
View All Lungs, Breathing and Respiration Articles
This tool is not intended to provide any medical advice. It is intended for informational purposes only. It is not a substitute for professional medical advice, diagnosis or treatment. If you find something that interests you on this website, it is important to seek professional medical advice before seeking treatment. If you believe you are experiencing a medical emergency call immediately your doctor.
Chest physiotherapy (CPT). Nursing Reviews.
Trendelenberg for chest physiotherapy. Children’s Hospitals and Clinics of Minnesota
Chest Physiotherapy Treatment (CPT). Cincinnati Children’s Hospital Medical Center.
High-Frequency Chest Wall Oscillation (the Vest). Cystic Fibrosis Foundation.
Abstract
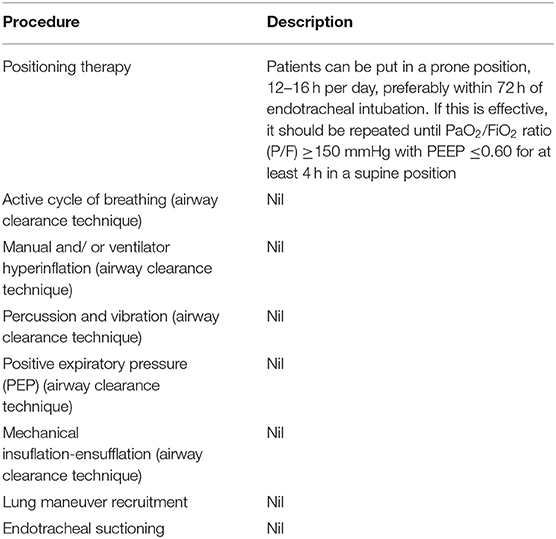
A beneficial adjuvant role of chest physiotherapy (CPT) to promote airway clearance, alveolar recruitment, and ventilation/perfusion matching in mechanically ventilated (MV) patients with pneumonia or relapsing lung atelectasis is commonly accepted. It is doubtful that routine CPT can be used in patients with no lung diseases. A literature review of prospective random trials that compared CPT to a non-CPT strategy for adult patients ventilated for 48 hours or more was conducted. Six studies were found. Sample size was small. Many CPT options were tried, including body positioning, manual manipulation of the chest (mobilization, vibration, compression and vibration), as well specific techniques such intrapulmonary and lung hyperinflation. General nursing care was provided to control subjects, as well as tracheal suction. In general, CPT was safe and supportive, yet had debatable or no significant impact on any relevant patient outcome parameter, including pneumonia. Current evidence does not support “prophylactic” CPT in adult MV patients without pneumonia.
Keywords: Chest physiotherapy (CPT); intensive care unit (ICU); mechanical ventilation; ventilator-associated infectious complications; ventilator-associated pneumonia (VAP).
Abstract
Background: This new chest physiotherapy method (CPT) to relieve infant respiratory symptoms such as bronchiolitis and syncytial viruses has been proposed. CPT includes 15 extended slow expirations and 5 provocated cough maneuvers.
METHOD: Twenty infants of average age 4.2 month were randomly divided into two groups. Eight patients received 27 sessions, while 12 received 31. These sessions included nebulization with hypertonic solution and our CPT technique. We utilized the Wang clinical severity scoring method (which evaluates wheezing. respiratory rate, retractions and general condition). S and heart rates were measured before and after each CPT session (T0), 30 minutes after (T30) and 120 minutes after (T150).
Results: The Wang score at T150 was lower than T0 at T0 (P =.008). T30 had a significantly lower Wang score (3.6 vs. 4.3 P =.001), while T150 had a significantly lower Wang score (3.7 vs. 4.3 P =.002). T150 had a significantly higher wheezing score than T0 (1. vs. 1.2), P = 0.02 in the first group. In the second group, Wang scores were lower at T30 (0.8 vs. 1.3,P =.001), T30 (0.8 vs. 1.3,P =.001), T150 (0.9 vs. 1.3,P =.001), T0 (0. vs. 1.3,P =.001), T0 (0.9vs.1.3,P = 1.3, P= 1.3,P = 1.3,P = 1.3,P =. There was a significant difference between the different groups. At T30, the overall Wang score improved significantly (P =.02), retractions P =.05, respiratory rate P =.001 and heart beat (P..001). T150 showed no significant differences in Wang scores between the different groups. At T30 (versus T0) the difference in percent gain between the groups was significant for Wang score (P = .004), wheezing (P = .001), and heart rate (P = .02). The daily baseline Wang score, T0, decreased in the new method-CPT group by a large margin (P =.002) during 5-hospital days. It did not decrease in the first group. There was no evidence of adverse events. They had similar average hospital stays.
CONCLUSIONS. Our CPT technique showed some short-term improvements in the symptoms of bronchial blockage seen in infants suffering from acute respiratory syndrome virus bronchiolitis.
Introduction
Infant viral bronchitis can be a life-threatening condition in the lower respiratory system. Bronchiolosis is characterised by severe inflammation, edema or increased mucus secretion, which can lead to hyperinflation, wheezing, and small-airway permeability. More than 10% of children are affected by bronchiolosis.
Unfortunately, most treatments for bronchiolitis only have limited efficacy. Current literature shows that CPT (conventional chest physiotherapy) does not have an effect on the outcome. This is especially true for those with long hospital stays or illness duration. But, there are new methods which show encouraging results. A 2-stage CPT technique for Belgium, developed by our group and recommended at a Paris conference in 2000, has been widely used.
First, a long slow expiration is required (in French: expiration lente prolongee). Second stage: Provoked cough.
It was not tested in a controlled study.
According to the Wang clinical severity score system, each variable is given a numerical value (Table 1) between 0 and 3. A maximum Wang score of 12 is considered to be the most severe. An increase in Wang scores indicates a worse situation. Mandelberg and collaborators found an increase in Wang score for infants who had acute viral pneumonia.
Another study that looked at viral bronchiolitis patients showed identical results in terms of safety and efficacy.
Wang Clinical Severity Scoring system. We evaluated the effectiveness of CPT (prolonged slow expiration, provoked cough) using albuterol with 3% NaCl hypertonic solution. This was based on the Wang score for infants hospitalized with RSV bronchiolitis.

Abstract
A beneficial adjuvant role of chest physiotherapy (CPT) to promote airway clearance, alveolar recruitment, and ventilation/perfusion matching in mechanically ventilated (MV) patients with pneumonia or relapsing lung atelectasis is commonly accepted. It is doubtful that routine CPT can be used in patients with MV who do not have such lung diseases. Based on literature searches for prospective randomized trials, six relevant studies were identified. Small sample sizes were found. Various CPT modalities were used including body positioning, manual chest manipulation (mobilization, percussion, vibration, and compression), and specific techniques such as lung hyperinflation and intrapulmonary percussion. Patients in control received general nursing treatment and tracheal suppression. CPT proved to be safe, supportive and had little or no impact on the outcome of any patient, not even pneumonia. Current evidence does not support “prophylactic” CPT in adult MV patients without pneumonia.
Introduction
CPT, or chest physiotherapy (CPT), is widely recognized as an essential component of respiratory care for mechanically ventilated (MV), critically ill patients. It can be used even when there are no signs of lung disease. Truly, intubation intracheal causes severe problems in the cough reflex and mucociliary functions. The result is sequestration of lower-airway secretions and imposition. This exposes MV patients to severe lung complications [i.e., ventilator-associated tracheobronchitis, ventilator-associated pneumonia (VAP), and lung atelectasis], prolongs the weaning process, and may increase mortality ( One of the key tasks of the intensive care unit (ICU) physiotherapist in MV patients is to facilitate removal of retained or profuse airway secretions aiming to reduce airway resistance, optimize lung compliance, and decrease the work of breathing. The ICU physiotherapist has a wide range of manual and automated breathing techniques. In spite of this theoretical benefit, CPT practice for this indication is far from standardized varying from as-needed airway suctioning over a more intricate “multi-modality” approach to physiotherapist-driven manipulation of the ventilator. When defining what “routine” daily physical therapy should be, it is important to consider the constant need for protocolized medicine, such as the creation of VAP prevention bundles specific for each unit.
.Chest Physiotherapy Cpt
Kent Chiro-Med Wellness Clinic
| Website | https://www.kentchiromed.com/ |
| Address | 563 Gladstone Ave, Ottawa, ON K1R 5P2, Canada |
| Phone | +1 613-508-0113 |
| Category | Physiotherapy Ottawa |
Beverly Physiotherapy
Car Accident Physiotherapy Winnipeg
| Website | http://www.beverlyphysiotherapy.com/ |
| Address | 747 Ellice Ave, Winnipeg, MB R3G 0B5, Canada |
| Phone | +1 204-774-8385 |
| Category | Physiotherapy Winnipeg |



















:fill(white)

