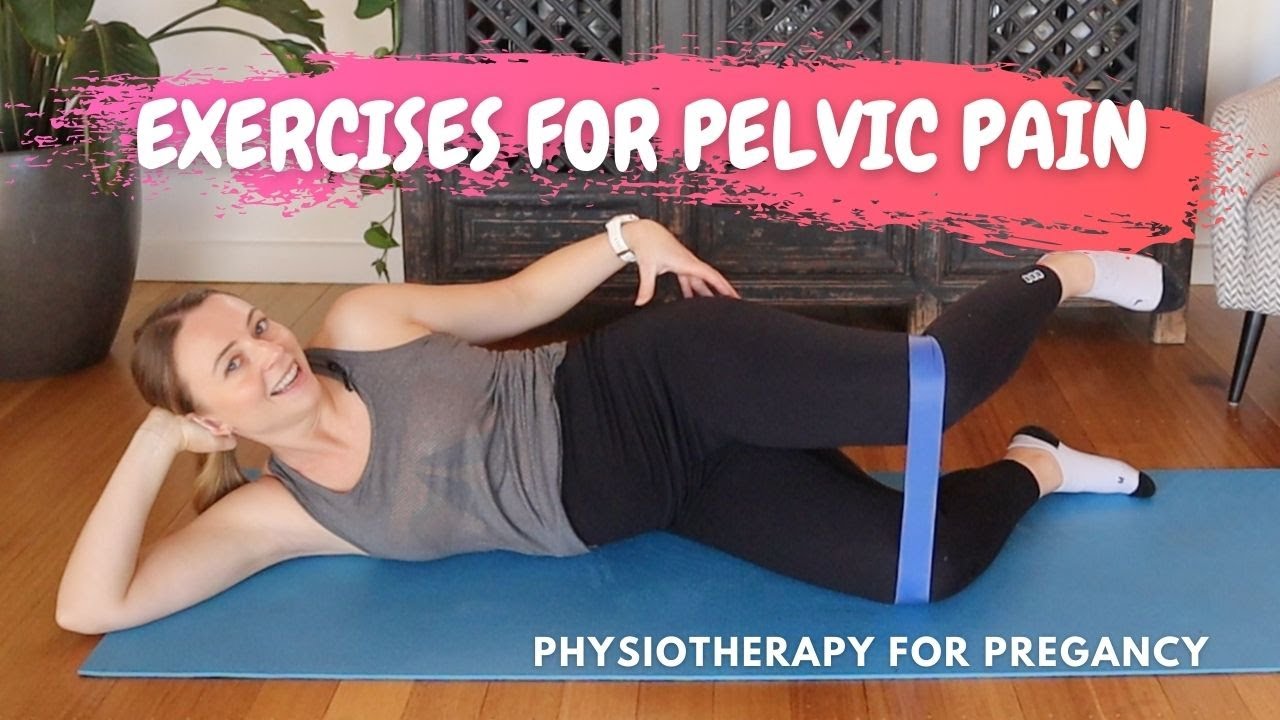
Physiotherapy For Pelvic Pain

Abstract
Introduction and Hypothesis: The complex condition of chronic pelvic pain in women (CPP), is not easily understood. Sometimes, the pain intensity and sensation do not correlate with the location of the lesion. They can also be experienced elsewhere. This may lead to sexual dysfunction (SD) and other musculoskeletal or myofascial disorders. These physical symptoms are common but are not well-underdiagnosed or treated. Patients often experience pelvic pain and psychological distress. This can lead to physical complaints. Doctors may prescribe medication or surgery to treat these symptoms. Often, however, the results are not satisfactory. It is reasonable to consider physiotherapy, as pelvic floor muscle problems are significant contributors to CPP and SD. The untapped and underutilized resource of physiotherapy can still be used in the multidisciplinary treatment of these health issues.
Methods. Both computer-aided search and manual searching were done for metaanalyses, systematic reviews (RCTs), and randomized controlled trial (RCTs), published in 1990 to 2017. These trials investigated classification, assessment, (physiotherapeutic, or physiotherapeutic, treatment) of pelvic pain, as well female SD, defined below. Interviews were done to get expert opinions.
Results: Due to a lack of sufficient relevant medical information, referral data, and test results, focused physiotherapy is difficult to administer adequately. But, quality research has shown that physiotherapy can have significant effects on female SD and CPP. Experts advocate for a multidisciplinary approach including physiotherapy.
Conclusions: Physiotherapy is a holistic treatment that can greatly contribute to multidisciplinary assessments and treatments of CPP/female SD.
Keywords; Chronic pelvic pain; Dyspareunia. Multidisciplinary. Physiotherapy. Sensitization. Sexual dysfunction. Vaginism. Vestibulodynia. Vulvodynia.
Introduction and Hypothesis
CPP is a complicated condition that affects women with chronic pelvic pain. It is common for pain sensation and intensity to not be related to the specific lesion, and instead are felt in other areas. This can lead metoskeletal and myofascial disorders (MSD) as well sexual dysfunction (SD). Although physical aspects are prevalent, they are often underdiagnosed and undertreated due to lack of understanding regarding its origin and distribution. Patients who experience pain in the pelvis often have psychological problems. The clinicians prescribe medication and surgical interventions to address these issues. However, this can sometimes lead to insufficient or no results. A physiotherapy approach is necessary because the pelvic floor muscle conditions are an important contributor to CPP or SD. The untapped and underutilized resource of physiotherapy can still be used in the multidisciplinary treatment of these health issues.
For meta-analyses and systematic reviews and random controlled trials (RCTs), published between 1990-2017, computer-aided searches as well as methodological quality assessments were conducted. These studies investigated classification, assessment and (physiotherapeutic treatment) of female SD. Interviews with experts were conducted to seek their opinions.
Due to a lack of sufficient relevant medical information, referral data, and test results, focused physiotherapy is difficult to administer adequately. But, quality research has shown that there are significant clinical effects for female SD and CPP. Experts advocate multidisciplinary physiotherapy.
Because it is holistic, physiotherapy has the potential to make a significant contribution in multidisciplinary treatment for CPP and female SD.
Introduction
CPP refers to abdominal pain beneath the umbilicus lasting at least 6 month [ ]. The complex, confusing problem can cause a loss of quality of life in women with multiple types of urogynecological problems [ ], and often causes depression, anxiety, or fatigue. CPP’s basis lies in the central nerve system. This causes emotional, cognitive and behavioral as well sexual reactions [ ]. CPP syndrome is CPP with no obvious infection. It is characterized as symptoms that are indicative of lower urinary tract and bowel dysfunctions (SD), [ ]. CPP syndrome (CPPS) is a condition in which pain intensity and sensation do not correlate with the lesion. It can lead to many musculoskeletal disorders, myofascial dysfunctions, SD, or other conditions. Peripheral sensitization is [ ]. Functionally “silent,” or functionally inactive fibers, may initially be activated if they are sufficiently stimulated by stimuli. This increases the excitability nociceptors. The release of neurotransmitters from the central terminals of nociceptors is initiated by electrical impulses. These signals propagate across synapses and dorsal-horn cells. Greater stimulus intensities are associated with greater release of neuropeptides, including substance P, from central terminals of C fibers. This leads to a higher postsynaptic responsiveness. This combination of intense afferent stimulation from viscerosomatic convergence and continuous somatosensorial inputs from muscle and skin at a dorsal segment of the spinal cord leads to central sensitization, which is perceived by the brain as intense, prolonged pain. The perception of central sensitization is allodynia or hyperalgesia.
A convergence of neural signals can sometimes hinder precise location and discrimination. It also forms the basis for referred pain and explains why visceral pathologies are commonly felt as pain in somatic structures innervated by the same spinal segment [pelvic floor muscles (PFM), in particular]. Furthermore, since visceral afferent fibers terminate over several spinal segments above and below the segment level of input, referred pain may be present in areas remote from the affected visceral organ. An increase in sensory system activity can also affect interneurons, which are connected to alpha, gamma, and typhoid motoneurons. It may cause spasm, overactivity, and contracture. This pelvic floor dysfunction and myofascial pain can then lead to SD, such as dyspareunia or vaginism, as the PFM tighten, becoming inflexible and incapable of accommodating penetration during intercourse.
Myofascial pain is an expression of dysfunction in the muscle and surrounding myofascial/connective tissue [ ]. Simons et. al. According to Simons and colleagues, myofascial symptoms are common in the elderly. The problem is still underdiagnosed and overlooked by physicians. The presence of myofascial trigger points (MTrPs) in the symptomatic region is a distinctive feature. There are two types of MTrPs: active and latent. Active points can cause pain by themselves and do not require stimulation. Latent points only feel painful when they are touched. Anatomical mapping can help you identify patterns of referred pain. MTrPs may also cause motor and autonomic disturbances, affecting the function of visceral organs [ ], are commonly found in many chronic pain conditions, and, when active, typically present as a regional pain syndrome [ Simons et al. [ ] MTrPs may be present in the pelvis as follows: anorectum (vagina), urethra and pubic bones, vagina, vagina, coccyxes, stomach, backside of legs, and lower back. It is possible that they may refer to pelvic pain, which can make myofascial pelvic discomfort difficult to locate [ ]. Dyspareunia and painful urination are common symptoms in myofascial pain. However, these symptoms can also be a sign of pelvic floor problems or other issues. Many authors report that in patients with CPP and/or SD the role of the pelvic floor is of the utmost importance [ ]. Dyspareunia in women suffering from overactive pelvicfloor has been identified in 57%. The symptoms are secondary to PFM stretching and stimulation. These symptoms, which can last up to three days, may have a significant impact on a woman’s physical health and quality of her life. They also cause feelings of anxiety and fear. Given the strong relationship between female SD and CPPS and PFM, it would be reasonable to expect that physiotherapy plays a significant role in treating these conditions. Relevant clinical practice suggests that physiotherapy may be an underutilized resource, which can decrease CPP or improve sexual function. This paper proposes that physiotherapy can be included in multidisciplinary approaches to treating women with CPPS/SD.
Types and models
To more reliably diagnose female SD, we consulted the American Physiatric Association’s (APA) Diagnostic and Statistical Manual of Mental Disorders 5 (DSM-V) of classified mental disorders with associated criteria [ ]. These categories include the psychogenic and natural causes of unwanted sexual behavior, desire and arousal. Although the APA recognizes that female SD for many women is physically disconcerting [ ], the DSM classifications are specifically limited to psychiatric disorders and are not intended to be used for evaluating or differentiating physical aspects of SD [ ]. Moreover, sexual disorders, such as dyspareunia and vaginism, are typically diagnosed independent of etiology, which may be largely or entirely physical in some instances.
Both vaginism and dispereunia fall under the umbrella of painful intercourse. They are both considered to be penetration disorders by the DSM V classification. This means that vaginal penetration with any method, including tampons or finger, is painful (dysparenuria) and impossible (vaginism). These conditions, which affect millions of women around the world [ ], are often not properly treated and underdiagnosed. Moreover, psychiatrists and psychologists find it difficult to differentiate between dyspareunia and vaginism [ ]. Dyspareunia is a condition that can be confused with vaginism. It occurs most often in cases of vulvar vestibulitis and vulvodynia. According to other literature, the incidence of female SD caused by chronic sexual and pelvic pains is between 7 and 58 percent [ ]. Another common type of vulvodynia is provoked vestibulodynia. It affects 12% [ ]. Vaginism is reported to affect up to 21% of women <30 years [ ], with an cumulative incidence of 10% of women unable to have sexual intercourse because of pain.
Gynecologists as well other medical professionals often concentrate on treatment and assessment of the peripheral manifestations of CPPS. Myofascial dysfunction and central sensitization are often overlooked, likely due to insufficient training [ ]. A decade ago, physiotherapy was virtually nonexistent for female SD and pelvic pain. There were very few reports on the subject. The well-known psychiatrist Rosemary Basson [ ] categorized the diagnosis and definition of major categories of women’s SD and their management. Vaginism is defined as persistent or recurrent problems in allowing vaginal access to any object, regardless of the woman’s desire. Management of Vaginism was solely based on behavioral factors, and not physiotherapy. In the case of dyspareunia they suggested treatment using cyclic-antidepressants. This could be used with or with out pelvic muscle physiotherapy. Important work by this group introduced the concept of a circular response cycle in women, termed the female sexual response cycle [ ]. Their study revealed that in addition to adequate sexual stimuli and motivation the woman’s emotional state and thought processes might also play an important role in the sexual reaction cycle. Women are most likely to become more sexually active and want to have sex more when they feel safe and secure. This cycle includes both psychological and physiological factors. The next question is why did they reduce the importance of physiotherapy in this cycle? New, emerging models see each individual as a social and psychosomatic entity. Each person is subject to complex interactions with both physical factors (genetics, biochemicals, etc.) and psychological factors (moods, personalities, behaviour, etc. The social factors that influence the individual (cultural, familial and socioeconomic), are also important. [ ]. Although this biopsychosocial model has been accepted in many disciplines (medicine, psychology, sociology), its prevalence and novelty differ across cultures. The model does however provide a useful tool for understanding and treating complex issues such as pelvic pain or female SD. These are often multifactorial.

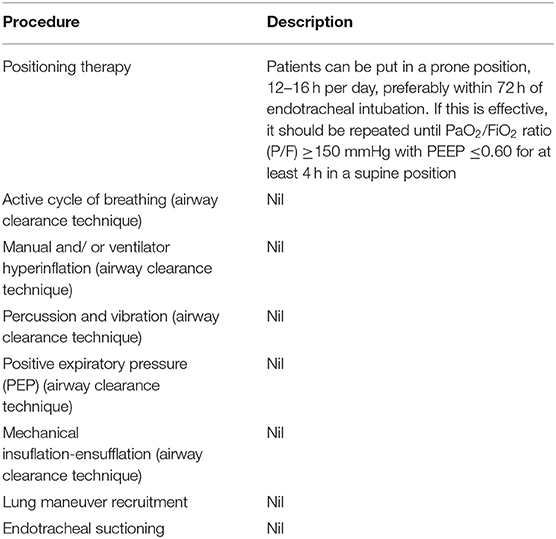
Table 1.
Inadequate Function or structural abnormality at an organ level
Deprivation of the ability to function/activate in a normal way
The ICF helps the physiotherapist influence pelvic pain and SD at three levels. Organ (impairment/disorder), personal (disability), and social-societal. While the DSM V concentrates on the psychological aspects at both the social and personal levels, with an emphasis on (changing inadequate) behavior, ICF includes organ levels that consider local physical disabilities and impairments. Element such as biological and psychological processing, sexual desire and arousal, motivation, and multiple motives for initiating or agreeing with sex require adequate psychological and physiological responses. Local pain or MTrP, overactive PFM, central sensitization-related hyperalgesia, and anxiety may hinder the state of mind around sex and/or sexual activity. The combination of psychological counseling and pelvic therapy may prove to be helpful in this situation.
Based on [ The female sexual response cycles (adapted from] Chronic pelvic pain can result from a weak and shortened PFM. This could be combined with reduced MTrPs, and restricted connective tissue. If spinal cord central sensibilization is not addressed, ongoing or unresolved injuries to the spine may result in dorsal roots reflexes that affect the spinal cord. These reflexes can cause symptoms such as urgency, frequency, and nocturia. This causes more pain, urgency frequency, and even nocturia. The result is further contraction/tension, which results in more restricted connective tissue and further reduction. [ ]. It is rare that a clinician would consider cystitis as a result of a pelvic floor injury. This could lead to central sensitization or dorsal root reflexes. Most likely, the clinician would continue the diagnostic process with invasive techniques or prescription of medication, rather than referring the patient to pelvic physiotherapy. Patients with severe morbidity include women with SD and pelvic pain. These patients are not only affected by pain but also have difficulty walking and maintaining normal daily life.
PFM dysfunction may be the cause of pelvic and female SD. Stress as the central factor provokes a vicious cycle, with pain leading to muscle tension, pressure, nerve entrapment, and reduced circulation, which results in muscle shortening, which leads to restricted movement, creation of MTrPs, and further pain as a consequence [ ]. There is no single cause for stress or pain. It can stem from multiple problems. CPP women have been through many failed therapeutic attempts that rarely provided adequate relief. These women require self-empowerment, according to key-opinion experts. Physiotherapy can play a critical role. It is not just the pelvic floor but the global impact of pain on the body. There are many other symptoms that can be caused by pelvic or musculoskeletal pain. Physiotherapy’s purpose is to help patients walk, stand and sit differently. Patients often notice a decrease in strain and a greater level of comfort as a result. The physiotherapist then can focus their attention on the pelvic area.
At the University College Hospital, London (UK), a multidisciplinary protocol was created with physiotherapy at its core. It has had high clinical efficacy rates and patients are satisfied with it. Personal communication by Dr. Sohier Elneil 2017. Physiotherapists need to be specifically trained and skilled in how to help patients avoid pain using cognitive and/or behavioral models, how to actively listen, and then how to display empathy for the emotional component of their patients’ disease [ In case of a referral to a pelvic physiotherapist, an accurate medical diagnosis is very important to determine the severity and impact of the disorder and to estimate success or failure of pelvic floor physiotherapy. In many cases, the presumed medical diagnosis (indication’) lacks accuracy, and physiotherapists are thus confronted with heterogeneity and unclear grade of severity, which may limit success or even result in failure. A lot of women who have dyspareunia, vaginism or other disorders experience high anxiety after undergoing a physical examination. This can lead to poorly diagnosed conditions [ ]. Studies from relevant science show that doctors failed to specify the location of pain in 93% and 44% respectively. They also did not address pathology in 74%, 74%, or pathology in 74%. In 95% of cases, there were additional criteria. Kavvadias et al. reviewed 69 studies and discovered that the pain site was not specified in 45%. Also, only 20% of doctors did a digital pelvic MTrPs exam for diagnosing [ ]. Focused physiotherapy is difficult because it lacks sufficient medical data, test results and referral information.
There is a recent tendency to more frequently involve physiotherapists in the multidisciplinary assessment and treatment of female SD and pain management. The University College Hospital 2017 has published multidisciplinary guidelines. The Pain Clinic of the University Medical Center Groningen Groningen (UMCG), Groningen in The Netherlands created the Pain Medicine Management Model. Instead of being assessed and treated by one specialist, as was the case in the past where the patient received treatment immediately after the assessment, new models use a multidisciplinary model that focuses on both the evaluation and the treatment. Through a multidisciplinary assessment, including a thorough history and physical exam, with additional testing/examination, as indicated, the team develops a comprehensive diagnosis that includes presumed pathophysiology of the (dominant) pain mechanism. The UMCG multidisciplinary pain center team consists of a medical team (urologist, gynecologist, surgeon), a psychologist (psychologist/psychiatrist/sexologist), and a physiotherapist. This team examines the predominant nociceptive (neuropathic), nonneuropathic; somatic, visceral and referred nervepathy. It also evaluates for peripheral and central sensitization, as well as any other provoking or perpetuating biochosocial factors. The assessment takes 1 h in each discipline. It is then possible to classify the patient and tailor the care plan accordingly.
Does Physiotherapy Help Pelvic Pain?
The use of physiotherapy as a treatment for chronic pelvic pain is increasing. This includes bladder pain syndrome, endometriosis and pudendal neurogia.
What does a Pelvic Physiotherapist do?
The pelvic floor physio has been specially trained to strengthen and rehabilitate the pelvic floor muscles. An endocrinologist, a specialist in medical medicine that deals with hormones and the body’s functioning, is an individual who can help you. May 28, 2017, 05:28
What’s the best exercise for pelvic pain
Kegel exercise is the most appropriate exercise to preserve your pelvic floor and avoid pain. Kegels can either be done lying down or standing. Juul 16, 2018.
What Happens At Physiotherapy For Pelvic Floor?
Your Physiotherapist takes a full history and will assess you. This will be followed by an external exam which commonly includes assessing posture, flexibility and strength around your low back, hips, and pelvis. A pelvic floor exam will be conducted afterward.
.Physiotherapy For Pelvic Pain
Kent Chiro-Med Wellness Clinic
| Website | https://www.kentchiromed.com/ |
| Address | 563 Gladstone Ave, Ottawa, ON K1R 5P2, Canada |
| Phone | +1 613-508-0113 |
| Category | Physiotherapy Ottawa |
Beverly Physiotherapy
| Website | http://www.beverlyphysiotherapy.com/ |
| Address | 747 Ellice Ave, Winnipeg, MB R3G 0B5, Canada |
| Phone | +1 204-774-8385 |
| Category | Physiotherapy Winnipeg |




















:fill(white)