Chest Physiotherapy Complications
What are the potential risks and complications of Chest Physiotherapy treatment?
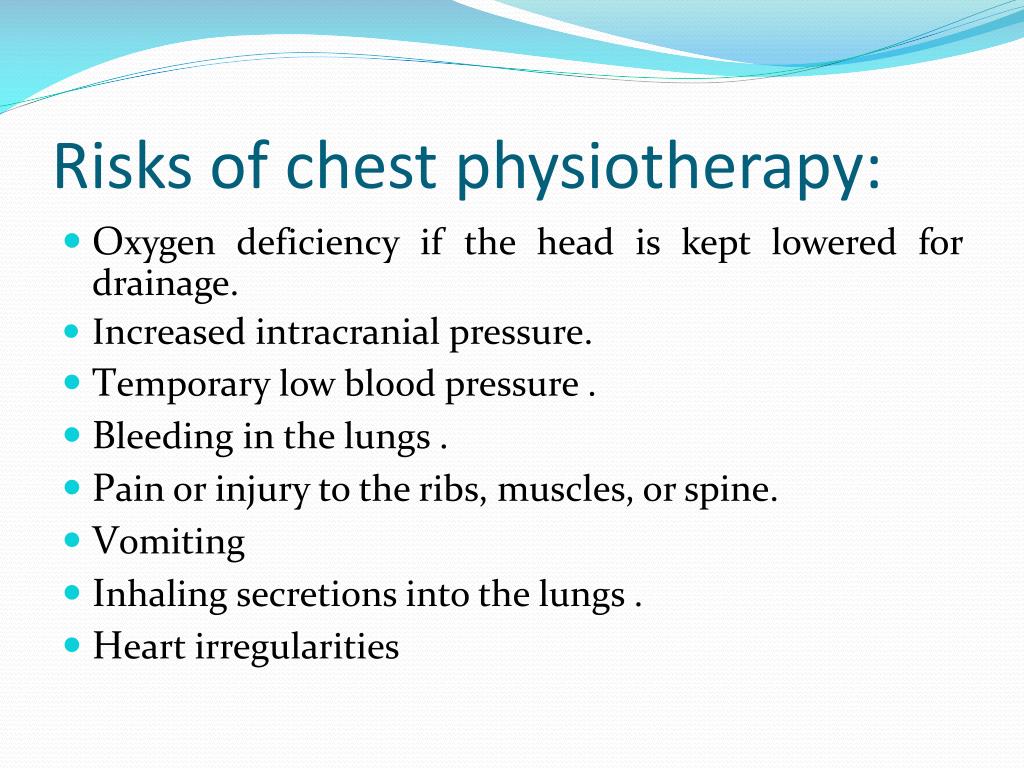
When the technique is appropriate to each patient, chest physiotherapy can be safe. The following complications can occur in chest physiotherapy:
Blood clots and blood arrhythmias Increased pressure in the head. Inhaling blood secretions. Low blood pressure. Spine pain. Vomiting. Certain individuals are more at risk for complications.
Blood thinning drug therapy (anticoagulants) Burns or other open wounds Inability to produce any secretions Certain respiratory conditions including asthma , bronchopleural fistula, pneumothorax embolism , and lung abscess heart attack high blood pressure Rib or vertebral fractures or osteoporosis Serious head or neck injury or increased pressure in the skull (intracranial pressure) Severe active bleeding (hemorrhage) Severe or uncontrolled pain Vomiting Reducing your risk of complications You can reduce the risk or minimize certain complications by telling your provider right away about any symptoms. Shortness of breathing, pain and headaches are common symptoms. It is also important to follow your treatment plan, including taking medications and breathing treatments as directed.
Similar Products
STEMI Watch – Diagnosis and Treatment of Pulmonary Problems After Upper Abdominal Surgery – PDF Download. Chest and pelvic physiotherapy can be used to prevent pulmonary complications. Inadequate pain relief, decreased functional reserve capacity and consequent decrease in PaO, delayed mobilization, diaphragmatic dysfunction, and other underlying conditions are all risk factors. Several methods of chest physiotherapy are available to avoid and treat postoperative pulmonary complications. It is difficult to determine the impact of chest therapy on patient outcomes, because chest PT is routinely given in many hospitals. In this paper, the effectiveness of chest PT in preventing postoperative pulmonary complications is reviewed, with focus placed on patients who have undergone upper abdominal and cardiac surgery.
Upper Abdominal Surgery. Lawrence and Associates evaluated the preoperative predictive value for postoperative lung complications. There were 22 actual studies on the predictive potential of preoperativespirometry. These studies all had flaws in the methodological analysis. They also found that there was an economic cost to hospitals due to the lack of accuracy of preoperative spirometry routinely for diagnosing postoperative lung complications. Further research is needed to confirm its positive impact on patient outcomes.
The hospital stay and incidence of cardiac and respiratory complications in abdominal surgery patients were also reported by the same team using a case analysis. This was done by comparing 96 cases with postoperative pulmonary complications to 96 control subjects. For these cases, hospital and ICU stays were considerably longer than that for the controls (24.1 days vs 10.3 days respectively) Heart problems and pulmonary complications are more prevalent than those with cardiac conditions. Longer hospital stays were associated with them (22.7 days vs 10.4). Incidences for the entire cohort were 9.6% (95% CI = 7.2-12.0) for pulmonary complications and 5.7% (95% CI = 3.6-7.7) for cardiac complications. According to this study, pulmonary complications were found more often than cardiac problems and associated with longer hospital stays.
Risk factors for pulmonary complications. Multivariable analysis was performed to assess the preoperative risk factors. Lawrence et al found that the Charlson comorbidity index (per point OR 1.6, 95% CI 1.004-2.6), Goldman cardiac risk index (per point OR 2.04, 95% CI 1.17-3.6), abnormal chest radiograph (OR 3.2, 95% CI 1.07-9.4), and abnormal findings on chest examination (OR 5.8, 95% CI 1.04-32) were associated with postoperative pulmonary complications. It was not established that preoperative spirometry and severity of COPD were useful for predicting postoperative lung complications.
Kroenke et al. compared the postoperative risk of pulmonary complications among patients with COPD. The prevalence of cardiovascular, pulmonary and vascular complications varied between groups, regardless if they had mild or moderate COPD. An analysis of logistic regression showed that complications after surgery were often related to perioperative complications such as high ASA scores, aging, and use perioperative bronchodilators.
McIntosh et al. conducted a metaanalysis of Chest PT Thomas and McIntosh. The authors searched for literature that examined the effect of various types of chest PT on the prevention and treatment of postoperative pulmonary complications. A meta-analysis of 116 articles was conducted. The common odds ratios (CORs) for the above interventions in preventing postoperative pulmonary complications were as follows. (See Table.) Table Efficacy of different chest PT modalities in preventing postoperative pulmonary complications # of Studies IS vs. No PT DBEX vs. No PT IS vs. IPPB IS vs. DBEX IPPB vs. DBEX Randomized Controlled Trials of Chest PT Recently, two RCTs of the use of chest PT in prevention of postoperative pulmonary complications were reported. Hall and his associates prospectively randomized 462 patients undergoing abdominal surgery to four groups. The risk of developing respiratory complications in patients who underwent abdominal surgery was 8%, 11%, 19%, 152, and 149, respectively. While there was no difference in the incidence of pulmonary problems between groups, the total time that the physiotherapist took to treat them was 17 minutes, 25 minutes and 55 minute, respectively.
Olsen (and associates) also performed a randomized prospective study. There were 174 patients who received chestPT. This included breathing techniques such as huffing and coughing while puffed lips, pursed lip breathing, and coughing. Seventy-four patients got no chestPT.7 However, the incidences postoperatively of pulmonary complications after surgery was 6.6% and 27.7% respectively. Although treated patients were mobilized significantly earlier, no difference in hospital stay was found between the groups.
Summary and recommendation Based on the information reviewed, you can make these statements. 1) Preoperative Spirometry is not able to predict postoperative lung complications. 2) Postoperative lung complications are more prevalent and have a longer hospital stay. 3) Common risk factors for pulmonary problems include a high ASA score, comorbid underlying illness (e.g. heart disease), aging and abnormal chest x-ray findings. These patients are a good target audience for chest PT. DBEX is more effective than any chest PT in the prevention of postoperative pulmonary complications. 5) Unfortunately, a new RCT didn’t prove IS superior to DBEX/IS + PT. Similarly, another RCT was unable to find any difference in hospitalization rates between chest PT and no PT. While it appears that certain patients could receive chest PT like IS and DBEX for their care, more RCTs will be required to show any benefits on cost and hospital stay.
Coronary artery bypass surgery Coronary arterial bypass surgery has become one of the most routine operations. This is because it is one among many common procedures performed across most industrialized societies. But, it is unknown what effect chest PT can have on outcomes and morbidity.
Randomized Controlled Trials for Chest PT stiller and his associates prospectively randomized 120 people into one of three groups. The first group received no PT, while the second received breathing and coughing exercises daily by a physiotherapist on their two most recent postoperative days. On the fourth and fifth postoperative days, the physiotherapist provided the intervention twice daily. Group 3 had the same interventions but with the frequency increased by 7.5%. The incidence, severity, or clinically relevant pulmonary complications of hypoxia, fever, chest xray abnormalities and chest hyperxia was not different between the two groups. Stiller et.al questioned routine coronary artery surgery’s prophylactic use of chest PT.

Introduction
CPT (Chest Physiotherapy) has been praised as an essential component of respiratory care in mechanically ventilated patients (MV) who have not yet developed significant or primary lung disease. Indeed, tracheal tube intubation can seriously affect the function of the cough reflex as well as mucociliary and escalator functions. It results in sequestration or impaction of secretions from lower airways. This exposes MV patients to severe lung complications [i.e., ventilator-associated tracheobronchitis, ventilator-associated pneumonia (VAP), and lung atelectasis], prolongs the weaning process, and may increase mortality ( One of the key tasks of the intensive care unit (ICU) physiotherapist in MV patients is to facilitate removal of retained or profuse airway secretions aiming to reduce airway resistance, optimize lung compliance, and decrease the work of breathing. The ICU physiotherapist has a wide range of manual and automated breathing techniques. In spite of this theoretical benefit, CPT practice for this indication is far from standardized varying from as-needed airway suctioning over a more intricate “multi-modality” approach to physiotherapist-driven manipulation of the ventilator. In determining the function of routine daily physiotherapy, one must consider both the ever-present need to protocolize medicine (e.g. creating unit-specific VAP prevention “bundles”) and the concerns surrounding medicolegal responsibility.
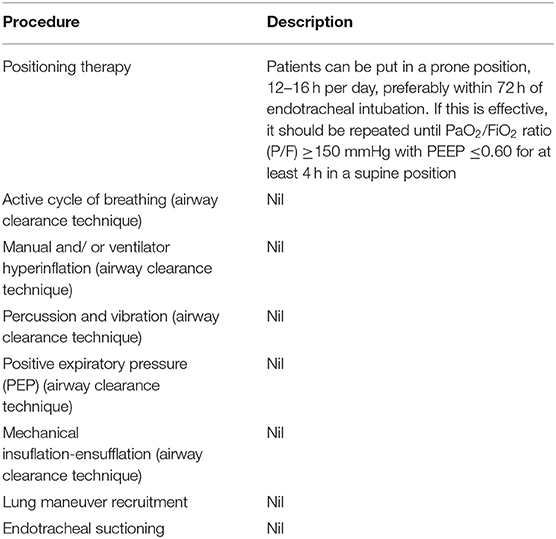
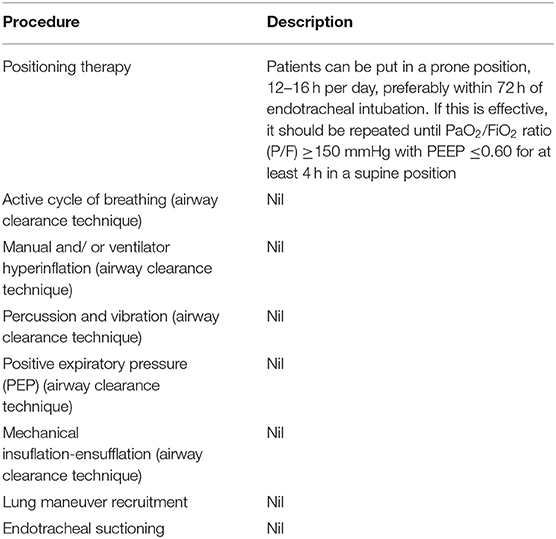
Table 1
Author Reference (refer) CPT interventions for patients
15 no CPT Mobilisation, suction; bid
15 IVP-AADP 20-minute IPV/AADP sessions. Suction.
CPT, chest physiotherapy; MLH, manual lung hyperinflation; VAP, ventilator-associated pneumonia; IPV-AADP, intrapulmonary percussive ventilation-assisted autogenic drainage physiotherapy; IVACs, infection-related ventilator-associated complications; bid, twice daily.
Ntoumenopoulos et al. studied 46 trauma patients ( ). CPT included postural drainage, manual lung hyperinflation, and two-times daily manual lung hyperinflation. 22 subjects participated. In comparison, patients in the control group were aspirated at least once per hour and remained on their beds. No difference was observed in VAP incidence and duration of ventilation. The same investigators subsequently focused on a mixed ICU population of medical, surgical, and trauma patients ( ). Two-daily postural drainage sessions were given to patients in the treatment (n=24) while those in control (n=36), were suctioned occasionally by nursing staff. CPT patients had less VAP as determined by their clinical pulmonary infection score (CPIS), P=0.01. There was no difference in the duration of ICU stay or ventilation from CPT and there were no adverse effects on mortality. There were two points of concern: the 17-year-older tracheostomized compared to 7 in the control, P=0.19 ( Templeton & Palazzo analyzed a sample of 172 hospitalized trauma patients [pooled specificity & sensitivity, respectively, of 0.65 & 0.64]. ( Templeton et al. CPT was used to treat 87 patients. It included body positioning, manual lung hyperinflation and chest wall compression, vibration, and suctioning. Aspirated from the 85 controls were those who had not been mobilized. The CPT-treated patients developed more VAP (35 vs. 25% controls; P=0.1). CPT also remained ventilator-dependent for longer periods (median, 15 vs. 11, days until extubation; P=0.041). ICU length of stay, mortality did not differ between the two groups. Some of the flaws found in this study were: a large time period (7 years) gap between study close and publication; inclusions of 17% patients with “respiratory fail due to infection”, a questionable randomization procedure, trends for greater tracheostomy usage, an increased severity level (P=0.10) as well as more organ failures (P=0.22) within the CPT group.
Gaude and Pattanshetty studied 173 patients in a medico-surgical setting (87 CPT vs. the 86 controls). ( ). Although the CPT method performed similarly to the other studies, the CPT was also comparable. However, the CPT control group had manual lung hyperinflation. VAP incidence and duration of ventilation did not differ between CPT and control patients. CPT subjects stayed longer in the hospital than CPT.
Patman et al. studied intensified CPT (i.e., six-times daily posturing, manual lung hyperinflation, and suctioning) in patients with cerebral trauma ( ). CPT was aspirated from seventy two patients and not the control group. VAP was initially defined by CPIS. If this score exceeded 7, then quantitative cultures could be obtained using non-bronchoscopic saline. Study results showed no differences in mortality, VAP incidence, ventilation duration, ICU stay and ICU stay.
CPT with intrapulmonary percussive ventilator (IPV), was the subject of two RCTs (). Clini et al. CPT and IPV were compared in 46 consecutive tracheostomized patients. They were offered CPT for one hour twice daily, CPT for a similar duration with two 10-minute intervals of IPV or CPT for the same time and two additional CPT sessions. During the 15 day-treatment period, the group that additionally received IPV (n=24) had less pneumonia (6 vs. 12 patients) and a progressive improvement in oxygenation and respiratory muscle performance. However, this study did not enroll ICU patients but patients referred to specialized “weaning units”. We were not able to specify the type of CPT or diagnosis of pneumonia. Importantly, the results of this study cannot be considered relevant to MV subjects because they were only available for patients with spontaneous unassisted breathing. Spapen et al. Spapen et.al. At study enrollment, all patients had normal chest X-rays and airways free of bacterial colonization or infection. Three groups were randomly assigned to patients. One group received CPT. The control was aspirated and mobilized to bed. CPT consisted of chest wall percussion and vibration twice per day, body positioning, suctioning and suctioning. CPT with IPV (20 minutes) and AAD (assist autogenic drainage) was also administered to a third cohort. The CPT sessions were performed 24/7 by 2 dedicated physiotherapists. All patients were treated with the same prevention steps for VAP. There were 45 patients enrolled, with each subject being 15 in each of the groups. Study endpoint was a documented Gram-negative infection-related ventilator-associated complication (IVAC), according to the Centers of Disease Control 2011 Working Group Guidelines ( ). One patient in the IPV–AAD study had Gram-negative IVACs, while the same number was found in seven other patients. A wide range of factors could have led to bias including heterogeneity among admission diagnoses, concurrent antibiotic therapy for nonpulmonary infectious diseases, different enteral nutrition policies and significantly younger patients being treated with IPV-AAD. There was also a poor correlation between IVACs and real VAP. Acute cerebral pathology was the predominant cause of half of patients included. This made evaluation variables like ICU stays or length of stay in ICU irrelevant.
Background
Cardiac and abdominal surgery are associated with an occurrence of pulmonary complications (PC), defined as any pulmonary abnormality that occurs during the postoperative period which produces identifiable disease or dysfunction that is clinically significant, and which adversely affects the clinical course [ ]. The location of surgery and whether there are risk factors, as well as the criteria for defining them. There is no single standard to describe PC in the postoperative period [ ]. These include postoperative infections, pneumonia and radiographic conditions such as infiltrates and atelectasis. PC’s high prevalence is due in part to altered ventilatory function. This is normal after surgery in the thoracic regions. Aelectasis can be complicated and could result from a number of factors including diaphragmatic dysfunction (diaphragmatic dysfunction), abdominal distension, chest wall changes, pain and chest wall modifications [ Coronary bypass surgery without or with extracorporeal circulation causes a severe impairment in respiratory system mechanics. CABG performed with CPB and off-pump CABG is no better than CABG done without extracorporeal circulation [ ]. There have been no randomized controlled studies that show the benefits of off-pump CABG. Postoperatively, atelectasis seems to be inevitable. [ Although respiratory physiotherapy has been used infrequently to treat or reduce PC after heart surgery, evidence is scarce to show their efficacy. The best therapy is not yet agreed upon. Postoperative breathing exercises are combined with physical therapy (CABG), to decrease atelectasis and other complications. Paskina, et al[] reviewed the evidence and concluded there was not sufficient data to prove the effectiveness of any prophylactic respiratory exercise after cardiac surgery.
While most of the literature discusses interventions that have been used after surgery, a number of studies also exist on the effect of preoperative physical therapy on reducing PC after cardiac surgery. In 2005, Westerhal et al. [ ] Researchers found that chest physiotherapy, which included deep-breathing exercises and preoperative physiotherapy, had a significant effect on reducing atelectasis as well improving spirometry. This was in contrast to the regime with no breathing instructions, following CABG surgery.
Others have also studied individual short-term preoperative interventions. In a small, non-randomized study, Rajendran et al. Rajendran, et. al. Castillo-Haas found that patients who were diagnosed with atelectasis after surgery had a significantly lower incidence than those who received postoperative chest physical therapy. They also noted that it didn’t have an impact on patients who suffered from respiratory problems as a consequence of infection.
It has been proven that preoperative physiotherapy can be used before abdominal and open heart surgery to decrease postoperative radiological and auscultation alterations and blood gas levels. [Recently, Hulzebos and al. In a random clinical trial, high-risk patients who underwent CABG surgery were found to have a lower incidence of PCs and shorter hospital stays after intensive inspiratory muscles training.
Some studies have confirmed the efficacy and safety of preoperative respiratory physiotherapy in preventing PC following CABG surgeries. However, there is no research on whether preoperative therapy has any effect on CABG operations that are not performed on the off-pump. This study aims to examine whether the frequency of pulmonary complications can be attributed to preoperative respiratory therapy in off-pump CABG patients.
.Chest Physiotherapy Complications
Kent Chiro-Med Wellness Clinic
| Website | https://www.kentchiromed.com/ |
| Address | 563 Gladstone Ave, Ottawa, ON K1R 5P2, Canada |
| Phone | +1 613-508-0113 |
| Category | Physiotherapy Ottawa |
Beverly Physiotherapy
| Website | http://www.beverlyphysiotherapy.com/ |
| Address | 747 Ellice Ave, Winnipeg, MB R3G 0B5, Canada |
| Phone | +1 204-774-8385 |
| Category | Physiotherapy Winnipeg |
























:fill(white)