Physiotherapy After Hip Surgery
Abstract
Purpose: The patient’s ability to complete their planned physiotherapy session after hip fracture surgery has been proposed as an independent predictor for achieving basic mobility independency upon hospital discharge. Although we have limited knowledge about factors that can limit mobility, it is possible to find out. This led us to examine patient-reported factors that may limit mobility, including limitations in the ability of patients to follow physiotherapy programs.
Methods: There were 204 patients who had suffered a hip injury in consecutive. (Mean (SD), age 80 (9.9), 47 were taken from the nursing home.) They were all treated with multimodal programs. To assess the patient’s independence in basic mobility tasks, such as getting into and out of bed and sitting-to stand-to-sit in a chair or indoor walking, the Cumulated Ambulation Score was calculated. Pre-defined limitations; pain, motor blockade, dizziness, fatigue, nausea, acute cognitive dysfunction and “other limitations”, for not achieving a full Cumulated Ambulation Score or inability to complete planned physiotherapy sessions were noted by the physiotherapist on each of the three first postoperative days. This was because the physiotherapist wanted to see how well patients had recovered their prefracture functional level.
Results: Hip fracture-related pain and fatigue were both the main reasons that patients could not reach an independent basic mobility level (>85%), or did not complete their scheduled physiotherapy treatment (>42%) over three days. Just 54% of the patients had reached their pre-fracture baseline mobility level at discharge, which was on average day 10.
Conclusion: Based on the patient’s perception, fatigue and pain are the most frequent limitations in not achieving independent basic mobility and not completing physiotherapy after hip fracture surgery. Multimodal peri-operative programs may be possible to further optimize for frail patients. Rehabilitation Implications Early mobilization after hip fracture surgery is crucial for patients to return to their pre-fracture functional level. Patients with hip fractures are most likely to not achieve an independent Cumulated Ambulation Score (or physiotherapy) within a short time. These reasons include fatigue, pain, or their habitual cognitive condition. Knowledge concerning postoperative fatigue is important for rehabilitation professionals and should contribute as an essential factor when planning physiotherapy.
Keywords: Limitations; Basic Mobility; E exhaustion; Hip fracture
Essential Rehabilitation
All things considered, it is easy to forget about joint replacement. It is usually offered as an option only when other treatment options fail to work.
The chances of making a full recovery and living a pain-free life afterwards are high, but rely on closely following your healthcare professionals’ advice. It is important to limit your physical activity in the immediate future. However, it’s equally important not to stop moving at all, and your team will get you up and walking as soon as possible, possibly on the same day as your procedure.
Successful rehabilitation requires physiotherapy. Although the NHS recommends that patients should receive at least six weeks of physiotherapy treatment after a joint or hip replacement, it is important to note that where people live, the extent of their physiotherapy will vary.
Researchers at the Universities of East Anglia and Bristol discovered the secret to the postcode lottery. The research examined data on more than 37,000 individuals who received hip or knee replacements in one year.
It found that patients in London and the north of England are most likely to have physio after a lower limb replacement, while those in the southwest are least likely to have the physio they need. This disparity is not explained by variations in patients’ condition before surgery, nor the degree of impairment or disability after it.

What Is Physio All About?
Roger Kerry, Roger Kerry physiotherapist, states that patients with problems after surgery are likely to have a lack of physiotherapy post-surgery or not get it at all.
He says that physiotherapy “helps restore people’s joints function and independence following surgery.”
“Without it, there is always the chance of delayed recover, or, worse still, the patient losing more function than before the surgery because they are unsure what they can and can’t do. Without proper rehabilitation, a patient could end up with more pain than they had before the surgery. A physiotherapist should direct a programme of rehabilitation for patients after knee and hip replacements. They will help them move in the right direction.
Kerry comments that “proper physiotherapy can help strengthen, improve balance, and reduce the chance of falling. It gives the patient the confidence and ability to recover their joint function, as well as the opportunity to return to sport or work, where applicable.” Research shows that balance, strength and mobility exercises are all effective in speeding up or improving recovery. You can choose to do resistance exercises or an aerobic exercise. These could increase your range of motion and be performed in a group or one-on-one. Hydrotherapy is a form of hydrotherapy that allows patients to perform set exercises in warm waters. This makes functional movement more accessible.
Researchers discovered, however that both the contents and availability of NHS physiotherapy were not the same.
2. After surgery, physical therapy can be used in the Acute Care Phase.
The average patient loses more than 50% of the strength of their fractured legs in just a few weeks, whereas patients with fractures to the trochanteric limbs are the worst affected. A number of studies have supported intensive physical therapy during the acute phase. This is because it speeds up recovery compared to delayed physical therapy which begins 3-4 days after surgery. Patients who received intensive physical therapy (3 sessions per day) during the acute phase of hospital were able to meet functional discharge criteria on average 10 days sooner than patients in the regular physical therapy (1 session). Without compromising safety, patients in the former group reported excellent program compliance. Some items of high-intensive physiotherapy cannot be done in all patients in the acute phase after hip fracture surgery.
Following surgery, several exercises will be recommended. Ankle pumps can be used to perform plantarflexion and dorsiflexion on the ankle. Kneeextension strength training of the fractured limb is feasible when started in the acute phase () . Additionally, Kronborg et al.
Assessment of the effects of progressive fractured-limb knee-extension strength-training session. The patient was sitting next to the mattress and used an ankle weight-cuff, while doing three sets with maximum load. No hip pain-related adverse events were observed. On average, fractured limb strength deficits decreased by 50% to 32%. The exercises are followed by straightleg raises. These exercises are designed to improve muscle strength and control the limbs, particularly gluteal muscles and quadriceps. However, you should consult your orthopedic surgeon to determine if such physical therapy is possible.
Ankle pumps. Ankle plantarflexion (left), and ankle dorsiflexion. (B) Knee extension strength training. In order to straighten their knees, they will need to tighten quadriceps while supine. (C) Straight leg raise. As the patient is supine the patient will tighten his quadriceps and flex the hip while elevating the extremity from the bed. Hold this position for between 5-10 secs. Then, slowly lower it.
3. Score Monitoring During Acute Care Phase
In order to accurately assess postoperative recovery, patients must return to the pre-fracture state. It is possible to predict postoperative rehabilitation’s functional outcomes by measuring preoperative activity levels and comparing these scores with the postoperative followup values. These scores can be continuously monitored in discharged patients. There are many scoring options available for the monitoring of acute care patients.
Cumulated ambulation scores can be used to assess patients who have suffered from hip fractures. It was created specifically for monitoring and planning activities in a daily acute hospital program of physiotherapy. This system provides basic mobility information. Modified mobility score (NMS) is a measure of pre-fracture functional levels. This score is simple to apply and can provide a prediction for mortality and rehabilitation outcomes. NMS can easily be determined immediately following hospitalization in order to determine the level of pre-fracture and later during outpatient care. A timed-up and go test (TUG) measures functional mobility. It calculates the amount of time that an individual takes to stand from an armchair, move 3m along a marked line on the floor, and then return to the chair. The test has been used worldwide in many studies and is useful for predicting the results of rehabilitation through the quantification of functional mobility. This test can be used to forecast the likelihood of falling. It is not possible to test patients who have been restricted from full weight bearing after surgery and those with impaired indoor walking (walking aids are allowed but not without assistance). TUG testing is done on the day of discharge. This can also be performed in an outpatient setting. Verbal pain scores, also called verbal ratings scales (VRS), are powerful tools for assessing pain experience. VRS only focuses on hip pain after a fracture. The VRS is less error-prone than the visual analogue, which can be dangerous for elderly patients. These scoring systems can be used to evaluate pre-fracture status as well as continuous evaluation of clinical outcomes post-operatively ().
Physical Rehab After Hip and Knee Replacements is So Vital
Osteoarthritis is most commonly seen in the hip and knee joints. This joint is subject to a lot wear over time. The cartilage protecting the bones from degeneration will gradually degrade. Hip or knee replacement surgery can be recommended if the condition is severe enough to make it painful.
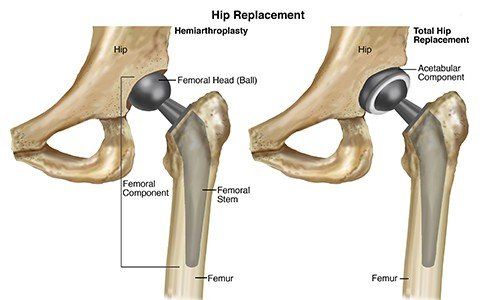
Canada has more than 100,000 patients who have had hip, knee and other replacements. Osteoarthritis is one of the main reasons for joint replacement surgery. The operation consists of the replacement of damaged parts of the joint with metal, ceramic, or plastic prosthetic pieces. The prosthetic should be fully healed after rehabilitation and can mimic normal function in the hip or knee.
But what about after the surgery?
It is essential to receive physiotherapy (which includes exercises rehabilitation) in order to get back to normal functions and enjoy the full benefits of your new joint. Initial rehab can be completed the day following surgery. For hip replacement surgery, it is common for healthcare professionals to have the patient up and walking or completing strengthening exercises the day after surgery. This helps prevent scar tissue from building up and allows for initial improvement in strength and range-of motion.
Aquafit Physiotherapy Clinic physiotherapists can guide you to a complete recovery. To track rehab progress, our experienced and trained physiotherapists will perform an initial assessment. This includes a baseline assessment and range of motion measurement.
Programs for joint replacement focus on strengthening around the joints and returning the joint’s full range to motion. To regain muscles and support the new joint, it is important to strengthen the muscles surrounding it. Hip replacement rehab targets the major leg muscle groups, the glutes, as well as the core muscles. When replacing a knee, the major leg muscles such as the quads or hamstrings, calves, and calf are important. They are responsible for the movement and functioning of joints.
Mobility exercises and range of motion help individuals return to their normal functions, which can prevent future injuries and pain. Most exercises are initially completed in a chair or on a bed, with the eventual progression to walking and weight bearing.
You may need to wait up to six weeks before you can return to regular activities for knee and hip replacements. The average recovery time from pain and swelling is 3 months. However, in certain cases it could take over a year.
Aquafit’s physiotherapists are here to help you. We can assist you in your recovery after hip, knee, or hip replacement surgery.
.Physiotherapy After Hip Surgery
Kent Chiro-Med Wellness Clinic
| Website | https://www.kentchiromed.com/ |
| Address | 563 Gladstone Ave, Ottawa, ON K1R 5P2, Canada |
| Phone | +1 613-508-0113 |
| Category | Physiotherapy Ottawa |
Beverly Physiotherapy
Car Accident Physiotherapy Winnipeg
| Website | http://www.beverlyphysiotherapy.com/ |
| Address | 747 Ellice Ave, Winnipeg, MB R3G 0B5, Canada |
| Phone | +1 204-774-8385 |
| Category | Physiotherapy Winnipeg |





















:fill(white)

