Chest Physiotherapy Vibration Machine

You might also be interested in similar products
AmazonBasics Corded Electric Handheld Classic Massager for Full Body(With Infrared)
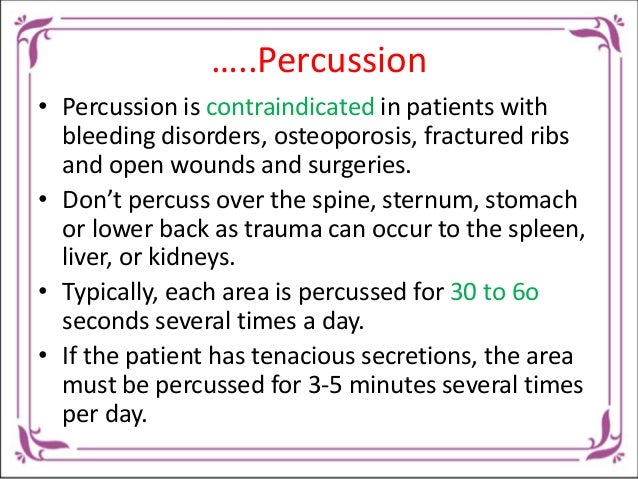
During chest physiotherapy. Vibration is one method used for postural drainage. This combination with chest drumming is used in therapy for COPD to remove mucus from the airways.
Items related to this product Page 1, 1 and 1
Description
Vibration Is Performed During Chest Physiotherapy. A fundamental method for performing postural draining, vibration is used. This technique helps to eliminate mucus buildup in the airways. It is also used with chestpercussion during COPD therapy. Vibration helps relieve COPD by gently shaking mucus and secretions into the large airways, making them easier to cough up. This is helpful because coughing is one of effective means of airway clearance.
Hom…

Positive Expiratory Pressure (Pep)
This valve increases resistance to exhalatory airflow in the mask/mouthpiece of PEP. Through the flow resistor the patient inhales and exhales 5-20 times. This creates positive pressure in their airways. A manometer can monitor and adjust the pressure. It is possible to choose between low and high pressures. The PEP mask/mouthpiece achieves the same goal as autogenic drainage (a special breathing technique aimed at avoiding airway compression by reducing positive expiratory transthoracic pressure) by expiring against an external airflow obstruction.
Most studies on the effectiveness of PEP have been conducted in Europe and they reported short-term equivalency of PEP to other methods of airway clearance. A published review of these studies found that PEP had similar effects on sputum clearance when compared with other methods (postural drainage forced exhalatory technique). One-year randomized controlled clinical trial comparing PEP with conventional physiotherapy for 40 children living with CF is the best evidence. PEP treatment led to improvements in lung function in the patients, while conventional physiotherapy caused a decline in this area. Statistics showed that the differences in FVC/FEV were statistically significant.
PEP Masks/PEP Valves can be found on the marketplace. You can find them here: Resistex PEP Mask, Mercury Medical, Clearwater, FL; TheraPep Valve, DHD Healthcare, Inc., Canastota, NY); Acapella (DHD Healthcare, Inc., Wampsville, NY); and PARI PEP Mask, PARI Respiratory Equipment, Inc., Midlothian, VA
The Intrapulmonary Percussive Valve (IPV), an aerosol machine, delivers pressurized gas minibursts at a rate of 100-225 cycles/min into the respiratory tract. Aerosolized medications are available under pressure. Oscillations that vibrate the chest can also be used. IPV permits continuous, monitored positive pressure applications and percussion through the whole respiratory cycle. This is in contrast with PEP and Flutter. Control of variables such as peak pressure, inspiratory duration and delivery rates is up to the patient. FDA grants Percussionaire status under 510(k).
There is a scarcity of scientific data to support the effectiveness of IPV. Homnick, et. al. (1995) conducted a study that found IPV effective in maintaining lung function. It was only 16 people. A study by Newhouse et al (1998) concluded that larger and longer studies of IPV compared to standard chest physiotherapy are needed to evaluate its value for independent administration of chest physiotherapy. There are not any studies that show IPV is better than pulmonary care at the hospital. Also, there have been no home-based studies.
Reychler et al (2006) stated that IPV, frequently coupled with a nebulizer, is increasingly used as a physiotherapy technique. Unfortunately, little has been done to study its clinical and physiological benefits. They compared lung deposition caused by amikacin using the IPV device nebulizer to standard jet (SJN) nebulizer. Amikacin were nebulized by both devices on a group consisting of five healthy people during spontaneous breathing. The deposition of amikacin was measured by urinary monitoring. Both devices had their drug output measured. The IPV device had a significantly lower respiratory frequency (RF), compared to SJN (12.6 +/– 2.5 breaths/min) p0.05. IPV had a significantly lower daily urine amikacin level than SJN (8.2 +/- 1.6 breaths/min versus 12.6 +/- 2.5 breaths/min, p > 0.001). Elimination half-life was identical with both devices. IPV output was less than SJN. While the amikacin delivery to the lungs was sixfold less with SJN than IPV, an even lower RF was used by subjects using the IPV. Researchers concluded that IPV was not suitable for the nebulization or administration of antibiotics.
Bruckner (2008) stated that assisted coughing and mechanical cough aids compensate for the weak cough flow in patients with neuromuscular diseases (NMD). In cases with preserved respiratory muscles, breathing techniques and special devices (e.g., Flutter or Acapella) can be used for secretion mobilization during infections of the airways. This physiotherapeutic approach can be described as oscillating therapy. Their mechanisms are dependent on separation of the mucus from the bronchial wall by vibration, thus facilitating mucus transport from the peripheral to the central airways. While their effectiveness is known in Mucoviscidosis (and chronic obstructive-pulmonary disease), there is little data about the impact on NMD. Simple oscillating therapies require a strong respiratory muscle force to be effective. The Percussionaire, i.e., IPV or high-frequency chest walls oscillation (HFCWO) are exceptions. It is evident that those with weak respiratory muscles can be over-strained by the application of these therapies or become tired. A general recommendation for the adoption of simple oscillating physiotherapeutic interventions can not be made in patients with NMD. Potentially, future HFCWO and IPV will offer greater effectiveness for NMD patients.
The Impulsator F00012 (Percussionaire Corp, Sandpoint, ID) is an intra-pulmonary percussive ventilator; it is a pneumatic device that delivers high-flow-rate bursts of air and aerosol to the lungs at a frequency of 200 to 300 cycles per minute. At a maximum pressure of 20 to 40% H2O, pulse breaths can be delivered. The pressure is titrated through visualizing the percussive movement within intercostal spaces. A mouthpiece delivers breaths and then the lungs are stimulated for 5 to 15 seconds over a 30-minute period. The effectiveness of Impulsator F00012 is not supported by evidence.
Kallet (2013) stated, “Many patients suffering from severe respiratory disease require special therapies such as inhaled medicine delivery to clear obstructions or treat pulmonary infection or stabilize gas exchange. Also, they may need to be ventilated to maintain their airway health and to enhance pulmonary hygiene. These therapies tend to be supportive, not curative. Currently, most lack high-level evidence supporting their routine use. In this overview, the author described the rationale and examined the evidence supporting adjunctive therapies during mechanical ventilation. The mechanistic, clinical and experimental evidence suggests that IPV can increase pulmonary secretion and may reverse atelectasis. But, it isn’t clear if IPV will have an impact on ICU stay and other outcomes. The most crucial issue is whether aerosolized antibiotics should be used to treat ventilator-associated pneumonia, particularly when caused by multi-drug resistant pathogens. Many studies show encouraging support for its use. Inhaled pulmonary vascular ligands provide only a brief improvement in oxygenation. However, they can be very useful for stabilizing pulmonary exchange in more complex circumstances. Uncontrolled, small studies indicate that aerosolized N/acetylcysteine and heparin may be able to reduce the severity of severe inhalation injury. Low-level evidence also suggests that heliox can be used to reduce airway pressure, improve ventilation and help with lower forms of obstruction. These therapies are usually supportive and could help patients manage their conditions. However, because they have not been shown to improve patient outcomes, it behooves clinicians to use these therapies parsimoniously and to monitor their effectiveness carefully.
Branson (2013) stated that postoperative pulmonary complications (PPCs) are common and expensive. With PPCs, the costs of hospitalizations and deaths are greater than for cardiac and thromboembolic conditions. PPCs are a main concern for respiratory therapists. This is done using many techniques such as continuous positive airway Pressure, chest physical therapy, incentive spirometry, IPV, and continual positive airway Pressure. This is despite the lack of scientific evidence.
What is Chest Physiotherapy and How Does It Work?
Chest physiotherapy refers to a range of physical exercises that can improve the function of your lungs and make it easier for you to breathe. CPT (Chest Physiotherapy) expands your lungs and strengthens your breathing muscles. It also loosens thick lung secretions and helps to drain them. The treatment of diseases such as COPD and cystic fibrosis can be done with chest PT. The lungs are kept clear during immobilization and after surgery to avoid pneumonia.
Only one treatment method for respiratory disease is chest physiotherapy. Chest physiotherapy is not the only treatment option. You may want to get an additional opinion.
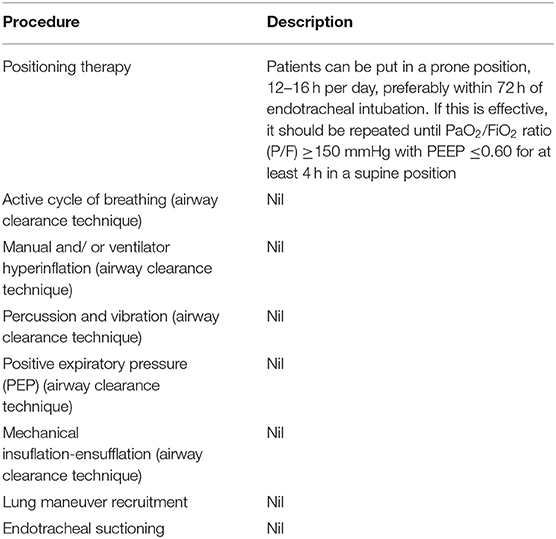
Chest Physiotherapy Types. Healthcare providers may combine several types of chest therapy, such as
Vibration and chest percussion are used to loosen lungs. A special CPT vest is worn by some patients, which can be connected to a machine. The machine makes the vest vibrate at high frequency to break up the secretions.
Controlled coughing techniques to help break up lung secretions so your caregiver can suction them out or you can cough them up.
Deep breathing is used to expand your lungs. To prevent and re-expand the lungs, it can also be used following surgery.
Positioning and turning from side to side to help improve lung expansion and drainage of secretions. This is important for patients who are bedridden or hospitalized.
The use of postural drainage to drain lung secretions. Other treatments that doctors might recommend Doctors may also suggest other procedures to treat respiratory diseases and problems. The severity of your condition, your medical history, and age all play a role in the treatments you choose. The following procedures and treatments for chest PT may be available:
What Is Vibration In Chest Physiotherapy?
To clear out secretions and phlegm from the chest, respiratory physiotherapists can use vibrations.
Does Vibration Help Pneumonia?
External mechanical vibrations of the chest were found to be a helpful therapeutic method in managing hypoxemia in patients suffering from atelectasis, pneumonia and other conditions. It was evident in an increase in PO2 and no changes in alveolar ventilation.
Can Vibration Loosen Mucus?
In addition to postural drainage, vibrating and shaking may also be an option. This will help loosen the mucous by shaking it loose. This helps to move the mucous from the smaller air sacs into the larger airways, where it can then be coughed up or suctioned.
Which technique is most effective for chest physiotherapy?
Chest physiotherapy can be prescribed twice daily, but with an increase in frequency when there are severe cases of bronchitis. Percussion, postural drainage is the most frequently prescribed.
.Chest Physiotherapy Vibration Machine
Kent Chiro-Med Wellness Clinic
| Website | https://www.kentchiromed.com/ |
| Address | 563 Gladstone Ave, Ottawa, ON K1R 5P2, Canada |
| Phone | +1 613-508-0113 |
| Category | Physiotherapy Ottawa |
Beverly Physiotherapy
| Website | http://www.beverlyphysiotherapy.com/ |
| Address | 747 Ellice Ave, Winnipeg, MB R3G 0B5, Canada |
| Phone | +1 204-774-8385 |
| Category | Physiotherapy Winnipeg |





















:fill(white)

