Manual Chest Physiotherapy

Manual Cpt or Vest Therapy
Manual CPT or chest physiotherapy using an airway clearing vest can be effective ways to mobilize mucus. However, there are important differences.
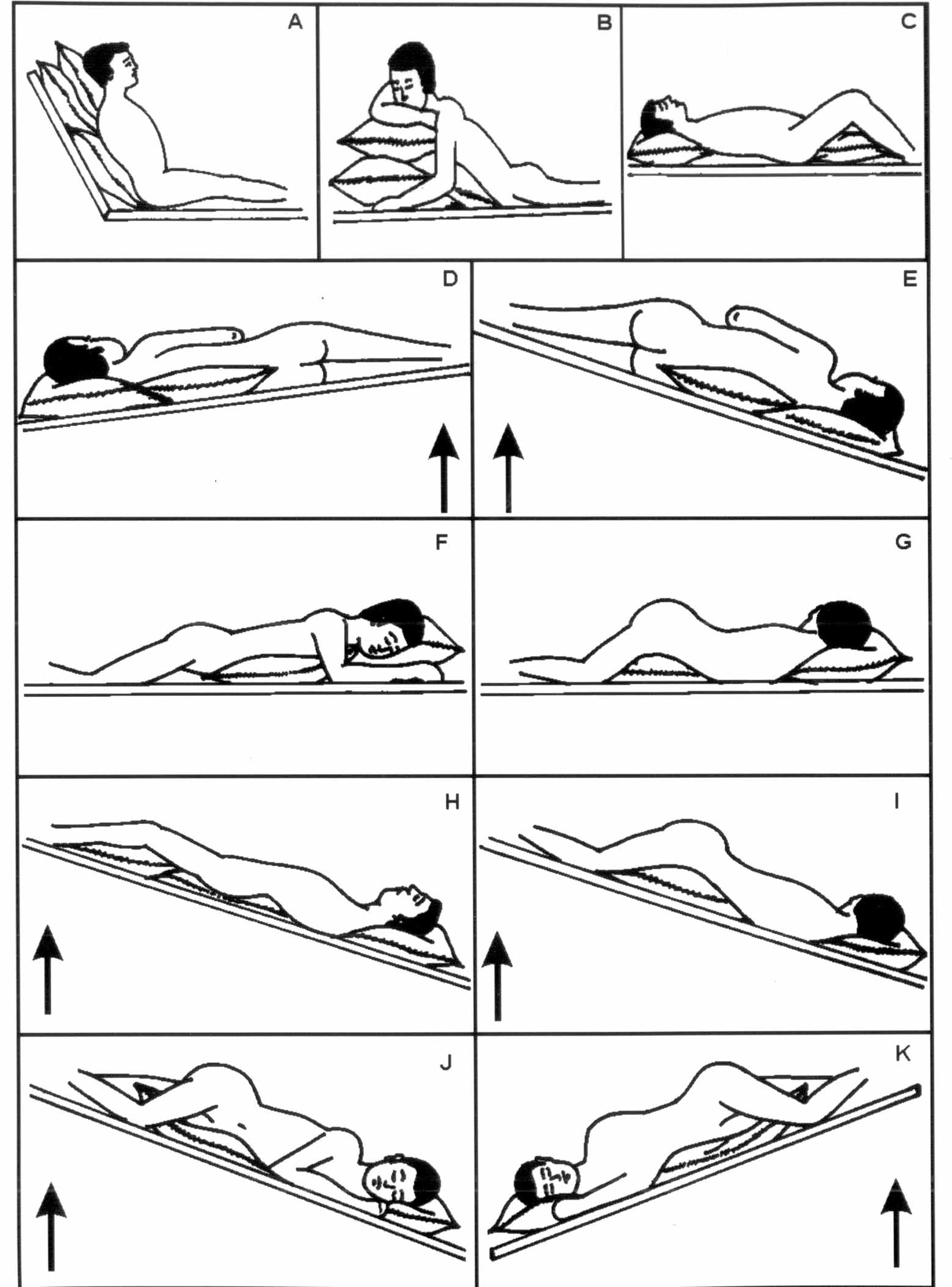
An essential difference between manual CPT and >percussion vest therapy is the latter can be performed independently. Manual CPT requires the use of gravity and assistance from a caregiver to drain mucus. Next, the caregiver uses gravity to loosen mucus from the chest and push it toward larger airways.
Allow airway clearing therapy to be carried out independently. Each therapy session can be administered by the patient using a SmartVest Airway Clearance System, which uses a high-frequency chest wall oscillation therapy vest (HFCWO). SmartVest provides rapid repeated pulses o air that quickly squeeze and release the upper bodies to move mucus away from the larger airways.
Abstract
Background: Manual chest physiotherapy (MCP) techniques involving chest percussion, vibration, and shaking have long been used in the treatment of respiratory conditions. However, clinical inequalities have resulted from limitations in research methods. Therefore, for patients suffering from an exacerbation or chronic obstructive pulmonary disease (COPD), it is based on clinical preference whether MCP should be administered. We standardized the administration of MCP, and evaluated its effect on disease-specific quality life.
Methods Patients were randomly assigned to either MCP or just advice about chest clearance. Six months after randomisation, the primary outcome was the Saint Georges Respiratory Questionnaire SGRQ (COPD-specific quality of life). Analyses were by intention to treat (ITT). ISRCTN13825248 registered this study.
Results: All patients had been included in the analysis. Of these, 372 (71%) provided the primary outcome data. As the threshold of superiority, an effect size of 0*3 standard deviations was established in SGRQ score. ITT analysis showed that there was no difference in SGRQ between patients who received or didn’t receive MCP (95 % CI: -0*14 to 0.19).
Conclusions: This data does not support routine MCP use in managing COPD’s acute exacerbations. However, it does not mean that MCP cannot be used in the treatment of COPD.

Similar articles
A randomised controlled equivalence trial to determine the effectiveness and cost-utility of Cross J. Elender F. Barton G. Clark A. Shepstone A. Clark A. Shepstone M. Blyth A. Bachmann M. Harvey I. MATREX Research Group. Cross J, et al. Health Technol Assess. 2010 May;14(23):1-147, iii-iv. doi: 10.3310/hta14230. Health Technol Assess. 2010. Clinical Trial. PMID 20487638
Effectiveness in integrating telemonitoring into existing hospital services upon admission for acute obstructive-pulmonary disease (COP): Randomized controlled study, blind, multicentre.
Pinnock H. Hanley J. McCloughan M. McCloughan A. Todd A. Krishan A. Lewis S. Stoddart A. van der Pol M. MacNee W. Sheikh A. Pagliari A. McKinstry A. Pinnock h. BMJ. 2013 October 17;347.f6070. doi: 10.1136/bmj.f6070. BMJ. 2013. PMC article free of charge Clinical Trial
The self-management of chronic obstructive and restrictive pulmonary diseases, which includes action plans for exacerbations.
Lenferink A, Brusse-Keizer M, van der Valk PD, Frith PA, Zwerink M, Monninkhof EM, van der Palen J, Effing TW. Lenferink A, et al. Cochrane Database Syst Rev. 2017 August 4th,8:CD011682. doi: 10.1002/14651858.CD011682.pub2. Cochrane Database Syst Rev. 2017. PMID: 28777450 Free PMC article. Review.
Phase 2a Randomised double-blind placebo-controlled study of Benralizumab in chronic obstructive lung disease (COPD) and sputum hemophilia.
Brightling CE, Bleecker ER, Panettieri RA Jr, Bafadhel M, She D, Ward CK, Xu X, Birrell C, van der Merwe R. Brightling CE, et al. Lancet Respir Med. 2014 Nov;2(11):891-901. doi: 10.1016/S2213-2600(14)70187-0. Epub 2014 Sep 7. Lancet Respir Med. 2014. PMC free article. PMID: 25208464 Clinical Trial
A brief educational program for patients about chronic obstructive breathing disease (COPD) can help you to develop action plans.
Walters EH Walters M. Walters R. Walters J. Howcroft M, et al. Cochrane Database Syst Rev. 2016 Dec 19;12(12):CD005074. doi: 10.1002/14651858.CD005074.pub4. Cochrane Database Syst Rev. 2016. PMID: 27990628 A free PMC article. Review.

Abstract
Techniques involving manual chest physical therapy (MCP), including vibration, vibration and shaking, have been widely used to treat respiratory issues. Unfortunately, the current research has limitations that have made it difficult to determine if this is a clinically appropriate treatment. Patients hospitalised for an exacerbation or chronic obstructive pulmonary disease (COPD) will have a preference as to whether MCP is used to help with sputum removal. We standardised the delivery of MCP and assessed its effectiveness on disease-specific quality of life.
In this randomised, controlled trial powered for equivalence, 526 patients hospitalised with acute COPD exacerbation were enrolled from four centres in the UK. Patients received MCP and advice either on their airway or on their chest. The primary outcome was a COPD specific quality of life measure, the Saint Georges Respiratory Questionnaire (SGRQ) at six months post randomisation. Analyses were performed with an intention to treat. ISRCTN13825248 registered this study.
The analyses included all patients, and 372 (71%) provided data that could be used to evaluate the primary outcome. As the threshold for superiority, an effect size of 0*3 standard deviations was established in SGRQ score. ITT analysis revealed no statistically significant differences in SGRQ scores for patients who had or did not get MCP (95%CI -0*14 – 0*19).
The data don’t support routine MCP use in COPD management for acute exacerbations. This does not necessarily mean MCP has no therapeutic value for COPD patients under certain circumstances.
Chest Physiotherapy During Mechanical Ventilation
The patient may not be able to breathe spontaneously if they are under mechanical ventilation. This can predispose the patients to developing lung collapse and ventilator-associated pneumonia. In such circumstances, chest physiotherapy can be used to reduce the length of stay in both a mechanical ventilator and ICU and prevent ventilator-associated pneumonia ( ). Additionally, patients intubated with high frequency chest wall oscillation had a higher dry sputum and PaO levels on day three. Lung collapse was reduced on days 2, 3 and 3. Culture positivity increased on day 3. Similarly, in a patient who received 11 sessions of physical therapy consisting of upright body positioning, mobilization and exercise, and the active cycle of breathing exercise technique every 2 h for 12 h over his 48-h stay in the ICU (six sessions on day one and five sessions on day two), arterial oxygen level improved markedly, with radiographic resolution of infiltration ( ). Chest physiotherapy is a treatment that reverses disease progression and reduces impedance in gas exchange. It can also be applied to patients who have COVID-19.
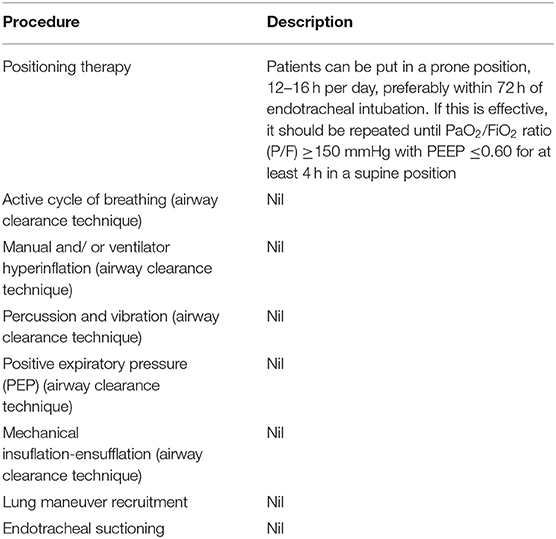
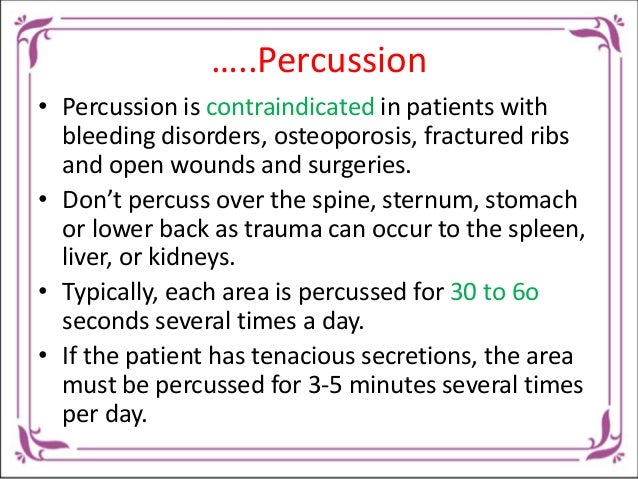
Airway clearance techniques, lung maneuver recruiting, endotracheal suckling, and change of posture are the recommended techniques for ventilator patients ( ). The airway clearance techniques recommended include positioning, active cycle of breathing, manual and/or ventilator hyperinflation, percussion and vibration, positive expiratory pressure (PEP), and mechanical insuflation-ensufflation ( ). There aren’t any details about how these techniques should be performed, except for positioning therapy. Also, no reports have yet been done on COVID-19 patients regarding the effectiveness of these techniques. You can see the details in Table 1 about positioning therapy. Additionally, you should exercise extreme caution with lung maneuver recruitment. Furthermore, chest physiotherapy during this period is indicated or contraindicated based on the status of the respiratory, cardiovascular, and neurological functions of the patients. Please refer to Table 2 for more details on contraindications and indications.
Abstract
Background Research Manual chest physiotherapy (MCP), techniques that involve chest vibration, chest percussion and shaking has long been utilized in treating respiratory problems. There is currently a lack of evidence to support this treatment due to methodological limitations. For patients with an acute episode of Chronic Obstructive Pulmonary Disorder (COPD), the clinical preference will dictate whether or not MCP is administered to aid with sputum clearing. We standardized the administration of MCP, and evaluated its effect on disease-specific quality life.
Methods In this randomised, controlled trial powered for equivalence, 526 patients hospitalised with acute COPD exacerbation were enrolled from four centres in the UK. The MCP was divided into two groups: advice on clearing the chest and airway, or both. The primary outcome was a COPD specific quality of life measure, the Saint Georges Respiratory Questionnaire (SGRQ) at six months post randomisation. Analyses were done with the intention to cure (ITT). This study was registered, ISRCTN13825248.
Results All patients had been included in the analysis. Of the 372 (71%) that provided valid data, the primary outcome was evaluable. As the threshold for superiority, an effect size of 0*3 standard deviations was established in SGRQ score. ITT analyses revealed no statistically significant differences in SGRQ scores for patients who had or did not get MCP (95%CI -0*14 – 0*19).
Conclusions. The results of these data do not support routine MCP treatment for COPD. This doesn’t mean that MCP has no therapeutic value for COPD patients, but it does indicate its potential usefulness in particular circumstances.
BMC Pulm Med. 2012;12(3) (c), 2012 BioMed central, Ltd.
Abstract
We measured the tidal volumes and peak inflation pressures generated during manual hyperventilation for chest physiotherapy in 25 adult ventilated patients. With a median (SD) value of 1120 (274 ml), the average tidal volumes ranged between 711 and 1511 ml. According to the Murray lung injury score, there was a negative correlation of the average tidal quantity and lung injury (p 0.05). Average peak inflation pressure varied from 37 to 74% cmHO with a median (SD) 51.5 (7.6) cmHO. The average lung injury score and peak inflation pressure showed a positive correlation (p0.05). The mean (SD) peak inflation pressure (Pa) was 18.3 (14.3) kPa higher than the baseline value after physiotherapy. (p 0.0.05). The mean (SD) of P a decreased by 0.4% kPa. Higher inflation pressures are applied to the lungs and lower tidal volumes, indicating an increase in risk for volutrauma.
Manual hyperventilation in chest physiotherapy has been well-established in ICUs. This technique was originally described in 1968. The goal is to expel excess bronchial contents [ ] and to reinflate the areas of atelectasis within artificially ventilated patients. There have been reports of improved gas exchange, increased lung compliance and reinflation of areas affected by atelectasis [ ]. Hyperinflation is not the only treatment for atelectasis. The use of chest vibration and positioning have been found to work better than just hyperinflation [ ]. There are disadvantages to this method of ventilation, including changes in oxygenation for patients with severe cardiac disease. Current mechanical ventilation methods are intended to prevent lung tissue from becoming too dilated [ ]. The high levels of inflation can result in barotrauma which causes significant increases in morbidity, mortality and other complications [ ]. So pressures need to be controlled to ensure adequate oxygenation. Extra-alveolar oxygen from lung injury secondary to intrathoracic pressure changes is called barotrauma. It has been shown in many animal studies that ventilation with high tidal volumes and high peak inflation pressures induces or extends lung injury [ Although controversial, peak inflation pressures > 35 cmH O are generally associated with increasing risk of barotrauma [ ]. A goal to reduce peak inspiratory forces to 30 cmH is shown to result in lower mortality. However, lung injury may occur at peak inspiratory pressures of 30 cmH O in normal sheep lung [ ] and with peak inspiratory pressures of 20 cmH O in rabbits whose lungs have been subject to saline lavage [ ]. It has been proven that barotrauma may be more common in patients with lung disease. A series of patients suffering from necrotising pneumonia had their peak inspiratory levels as low at 30 cmHO. Murray et al. formulated the lung injury score. as a means of grading the extent of pulmonary damage [ ] (Appendix 1).
We examined the ventilatory characteristics of mechanically ventilated patients under routine manual hyperventilation (for chest physiotherapy) during routine manual hyperventilation. Potential correlations were investigated between peak airway pressure and the tidal volume, as well as lung injury scores.

These are the methods
This was done with approval from the local ethics commission. Each patient had to give informed consent. We studied 25 sedated, mechanically ventilated patients aged 20-79 years who had an arterial cannula in situ and who were undergoing chest physiotherapy as part of their normal treatment. There were no patients with arterial cannulas, and patients whose lungs were being provided ventilation using either pressure-assist (or spontaneous) modes.
The Datex Capnomac Ultima monitor was used to measure the patient before, during, and after treatment. This was connected to a standard Mapleson C circuit as close as possible to the tracheal or tracheostomy tube. Regular calibration of the monitor according to manufacturer’s guidelines was done. These conditions result in the monitor’s pressure measurement accuracy of +- 1.5 cmHO and tidal volume accuracy of +-30 ml. Both the Datex Capnomac (and the patients’ ventilator) measured peak inflation pressures for the first 10 consecutive breathings. They were both compared to make sure that the readings were comparable. A physiotherapist performing manual hyperventilation wasn’t aware of the purpose of this study, so he was asked to do the procedure the same way.
Initially, the patient received artificial ventilation. For 10 consecutive breathes, peak pressures and tidal volumes were measured. Inspired oxygen concentration, positive expiratory pressure (PEEP), arterial carbon dioxide tensions and positive oxygen concentration were all recorded. We also noted the patient’s diagnosis, lung injury score, and size of their tracheal tube. Data were collected over 10 manual “breaths” beginning at expiration of first manual “breath”. Patients who received less than 10 manual ‘breaths were not eligible for the study. The physiotherapy ended with measurements of arterial oxygen and carbon dioxide tensions. A further 10 breaths of data were also taken when the patient was reconnected to ventilator, using the same settings and manual hyperventilation. We calculated the means for each set. Statistical analysis was performed using the Pearson correlation and the Student’s pair t-test. A statistically significant p value of 0.05 was taken to be significant.
Results
There were 19 male and seven female participants. We found that the average age for all patients was 47 (SD), years. The majority of patients were fitted with tracheal tubes, with an internal diameter ranging between 7.5 and 9.0mm. Two of the patients were fitted with tracheostomies. One had an inner diameter of 8.0 mm while the other one was 9.0 mm. The mean (SD, 0.83) lung injury score for the patients was 1.6. The average (SD) volume of manual hyperventilation was 170/36% of that delivered by patients’ ventilators before they received chest physiotherapy. The mean peak inflation pressure ranged between 37 and 75 cmHO, with an average (SD), of 51 (7.6)cmHO, and there was statistically significant negative correlation with the lung damage score (Fig. 1 ). With a mean (SD), of 59 (6.7) cmH O., the maximum inflation pressure was used was between 48 and 78 cmH. O. The pressures were determined using a disposable Mapleson C circuit with a valve that allows for a maximum of 60 cmH. This showed that the non-significant positive correlation was not evident with lung injury scores. These correlation coefficients are + 0.49, p 0.05 and + 1.35, p > 0.0.05 for the maximum and average inflation pressures.
Diagram showing the plot of the peak inflation pressure of 25 patients. Also, the sum of all the lung injury scores. Line of best fit also shown.
Manual hyperventilation used an average of 711 to 1511ml of tidal volume, and a median (SD) value between 1120 and 274 ml. The lung injury score had a statistically significant negative relationship (Fig. 2 ). Maximum tidal volume ranged between 838 and 1674 ml with a mean (SD of 1343 (236),ml). There was also a statistically significant negative correlation. The correlation coefficients measured were – 0.51 (p < 0.05) and - 0.65 (p < 0.05) for the average and maximum tidal volume, respectively.
Figure 1: Plot showing the average of 25 patients’ tidal volumes and the sum of all the lung injuries. Also shown is the line of best fitting.
On a 100% oxygen basis, oxygenation increased by a mean of 18 (SD18) kPa (p 0.0.05). 3 ). Number 24 was the only patient to experience a decrease of P a with manual ventilation. A patient with high lung injury scores of 3.3 and 4 was treated on 13 cmHO of PEEP. But, the statistically significant difference in ventilation (as measured by carbon dioxide tension) was not evident. There was a decrease in the mean (SD), P a of 0.4% (p >0.05).
Oxygenation levels of patients before and during chest physiotherapy. These data were for every patient, before and after (squares) physiotherapy.
.Manual Chest Physiotherapy
Kent Chiro-Med Wellness Clinic
| Website | https://www.kentchiromed.com/ |
| Address | 563 Gladstone Ave, Ottawa, ON K1R 5P2, Canada |
| Phone | +1 613-508-0113 |
| Category | Physiotherapy Ottawa |
Beverly Physiotherapy
| Website | http://www.beverlyphysiotherapy.com/ |
| Address | 747 Ellice Ave, Winnipeg, MB R3G 0B5, Canada |
| Phone | +1 204-774-8385 |
| Category | Physiotherapy Winnipeg |




















:fill(white)

