Chest Physiotherapy For Cystic Fibrosis
The Plain Language Summary
Chest physical therapy compared to no-chest physiotherapy.
Question: Review. The evidence was reviewed to determine if chest physiotherapy is more effective than no physiotherapy at clearing mucus from the lungs for people living with cysticfibrosis.
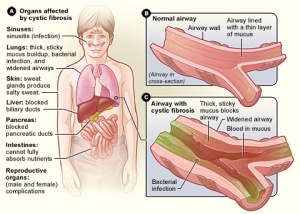
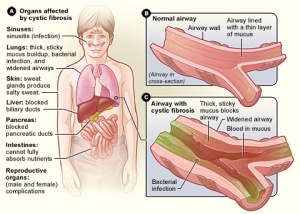
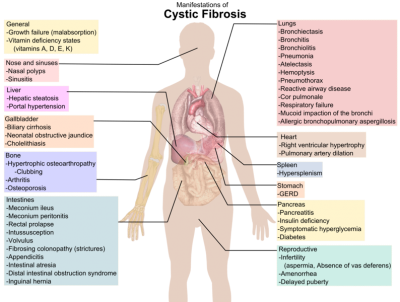
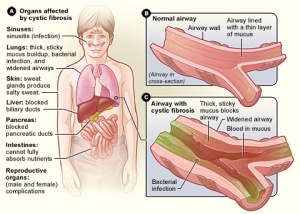
Background The lungs of people with cystic fibrosis produce excess mucus. It can result in repeated infections and tissue damage to the lungs. Clearing the mucus with drugs or chest physiotherapy is crucial. Physiotherapy clears mucus by different techniques or by using mechanical devices or both. Daily physiotherapy requires a lot time and effort. Therefore, it’s crucial to find out if it actually works. Our search for studies found that participants had the same chance of either being part in the chest physiotherapy group or not. This revision is an update to previously published reviews.
Date Search The evidence can be found at: 02 June 2015
Characteristics of the studies We reviewed eight studies that reported results for 96 patients with cystic Fibrosis. There were many studies that looked at several treatments, some compared with none. One looked at autogenic, six examined traditional chest therapy, seven assessed positive expiratory and oscillating pressures, one evaluated high pressure positive expiratory, and the other studied conventional chest physical therapy. The results could not be combined to make statistical analysis.
We summarize the key findings from these studies and conclude that clearing your airways has short-term benefits in moving mucus. Three studies measured sputum which had been coughed up and found those people using chest physiotherapy coughed up more sputum; four studies measured radioactive tracer clearance and found increased clearance with chest physiotherapy. The only study that reported improvement in lung function was one. Three other studies, however, did not show any effect of chest physiotherapy. The evidence for long-term chest physiotherapy effects has yet to be established.
Quality of the evidence Most of the included studies had some design problems which may affect confidence in the results. Only half of all studies did not report the entire results.
The physiotherapist and the patient will be aware of which treatment is being used in physiotherapy research. This may impact some findings. The amount of sputum gathered and the results of lung function tests were examined in half of the studies. A quarter of these questions asked the participants their opinions on the treatment. These findings may have been affected if they weren’t aware that the treatment was being used. None of the studies revealed whether the subject was competent in carrying out this treatment. This may affect how well they were able to do the treatment which could affect confidence in the results.
Abstract
BACKGROUND–Autogenic drainage has been suggested as an alternative method of chest physiotherapy in patients with cystic fibrosis. In this study autogenic drainage was compared with the active cycle of breathing techniques (ACBT) together with postural drainage. METHODS–Eighteen people with cystic Fibrosis participated in a two-day randomised crossover trial. Two sessions were given each day of autogenic drainage and ACBT. Each study day was one week apart. Patients were then monitored every day for six hours. Mucus movement was quantified by a radioaerosol technique. The airway clearance was assessed qualitatively with xenon133 scintigraphic tests at the beginning and end of every day. After each session, expectorated sputum were collected for approximately one hour. Each session was followed by a test of the lungs. Oxygen saturation (SaO2) and heart rate were measured before, during, and after each session. RESULTS–Autogenic drainage cleared mucus from the lungs faster than ACBT over the whole day. As determined by the xenon133 ventilatory studies, both methods improve ventilation. There were no overall differences in the results of the pulmonary function tests. However, more patients showed an improvement in forced expiratory flow, which ranged from 25% to 75% for autogenic drainage while others had an increase in forced vital capacity (ACBT). There were no differences in the sputum weight, heart rate or mean SaO2 between patients. However, four of them desaturated after ACBT. CONCLUSIONS–Autogenic drainage was found to be as good as ACBT at clearing mucus in patients with cystic fibrosis and is therefore an effective method of home physiotherapy. People with cystic fibrillis need to be evaluated in order to decide which type of treatment suits them the best.
References
Lechtzin N, West N, Allgood S, Wilhelm E, Khan U, et al. (2013) Design and Rationale for a Randomized Trial to Assess Lung Function and Electronic Symptom in Home to Diagnose Cystic Fever. Early intervention in the cystic fibrosis exacerbation trial. Contemp Clin Trials 36(2): 460-469.
Flume PA, Van Devanter D (2012). State of Progress in Cystic Fibrosis Respiratory Disease Treatment. BMC Med 10,88: 2-3.
Daniels T. (2013). Physiotherapeutic management techniques for cystic fibrosis treatment in adults. J Multidiscip Healthc 3 : 201-212. Main E. Prasad A. Van der Scheans CP (2005) Chest physiotherapy is more effective than other procedures for cystic fibrosis. Coch Database Syst Reviews 25(1): CD002011. McKoy NA and Saldanha IJ. Odelola OA, Robinson KA. (2012) Active cycle for cystic fibrosis. Coch Database Syst Reviews 12: CD007862.
Prasad SA. Tannenbaum E. Mikelsons CT (2005). Physiotherapy for cystic Fibrosis. JRSM93(Suppl. 38): 27-36.
Pryor JA, Tannenbaum E, Cramer D, Scott SF, Burgess J, et al. (2006) A comparison of five airway clearance techniques in the treatment of people with cystic fibrosis. J Cys Fib 5 : 76.
Mcllwaine, Peacock, D and Wong LT (2005) A long-term comparison of oscillating positive expiratory (flutter), physiotherapy for cystic fibrosis. J Pedi 138(6): 845-850.
Costantini D, Brivio A, Brusa D, Delfino R, Fredella C, et al. (2005) Postural drainage for CF infants: a long-term, comparative study. Pedi Pulmonol Suppl 22: 308.
Fainardi V, Longoa F, Faverzani S, Tripodi MC, Chettab A, et al. (2011) The Short-Term Impacts of Positive Expiratory Pressure and High-Frequency Chest compression in Cystic Fibrosis Patients. J Clin Med Res 3(6). 279-284.
Elbasan A, Tunali N. Duzgun I. Ozcelik U. (2011) Effects chest physiotherapy and exercise on children with cystic Fibrosis. Ital J Pediatrics 38: 2.
Abstract
Cystic fibrosis, a predisposed genetic disease that can cause difficulty in clearing bronchial segments, is known as CF. In addition to medicine different physiotherapy treatment techniques for instance postural drainage, percussion, chest shaking, huffing and coughing helps to clear bronchial sections and lessen the work of breathing. An absolute diagnosis and dosage-based chest physiotherapy are required. A CF patient’s livelihood depends on evidence-based physiotherapy.
Abbreviations : CF is Cystic Fibrosis. PEP stands for Positive Expiratory Pressure.
RIS APA Harvard IEEE MLA Vancouver Chicago Scroll
What Are the Treatments Available For CysticFibrosis?
Treatment for cystic fibrosis focuses on both lung health Treating Lung Problems Doctors will focus on preventing lung infections. CPT is also known by percussion and postural drain and loosens the mucus in your lungs. CPT involves the placing of the individual in a position that promotes drainage. After this, all areas of their lungs are “percussed,” by using a cupped arm to clap on their backs. CPT may be administered by relatives to small children. However, it is also possible for older and more experienced children to perform the procedure. CPT can be performed two times per day. However, it is possible to do more often if the patient has an active lung infection. Treatments using vibrating vests are also being widely used and appear to be better in many children, though expensive.
It is important to exercise to help reduce the secretions in your lungs.
To help someone cough up mucus, they can use mucus thinning drugs.
Inflammatory drugs can lower the inflammation levels in your lungs. Symdeko contains Tezacaftor/ivacaftor. This medication is available as a tablet and can assist in the movement of air through the lungs. This medicine is available to anyone 6 years and older.
Treatment of Digestive Problems. People suffering from CF must eat a balanced, high-calorie and high-protein diet. As children with CF, their ability to absorb nutrients is often reduced. This means they have to consume up to 150% daily to ensure that they meet their developmental needs. Multivitamins and supplements vitamins A, D, E, and K are also important. Cystic Fibrosis patients should consume pancreatic enzymes at every meal. Extra enzymes are needed to digest high-fat foods. Some people with severe digestive problems may need special high-calorie formulas that are administered through tubes or veins.
Gene therapy attacks the cause of cystic fibrosis rather than just treating the symptoms. Kalydeco or ivacaftor, which treats cystic-fibrosis by targeting the cause, is an exciting advancement. Kalydeco, which treats the particular gene defect found in four percent of patients with the condition — approximately 1,200 individuals in the U.S. For people aged 6 months or older, the drug has been approved.
Trikafta is a combination of ivacaftor (elexacaftor) and tezacafto (tezacafto). It is approved for patients ages 12 years and older.
Cystic Fibrosis patients may have needed a transplant to their lungs.
Abstract
One hundred and fourteen patients were treated for cystic fibrillis using self-administered PT techniques. These included autogenic drain (AD) or high-pressure PEP-mask (PEP). After visiting the clinic five days in succession, they performed the following: AD PEP, AD PEP followed with AD (PEP/AD), AD PEP (AD–PEP), AD PEP (AD–PEP), and then no PT except when there was spontaneous coughing. Lung function was continuously measured prior, during, as well as after PT. Time required and the amount of sputum produced each form were recorded. PEP was the best at producing sputum. PEP-AD, AD/PEP and AD were next. None of the four forms produced as much sputum as coughing. PEP/AD, PEP/AD and PEP/AD made significant improvements to lung function. But, PEP-induced changes weren’t as impressive as AD-induced ones. PEP-induced improvements in lung function were significantly less for patients with asthma. PEP-effected bronchospasm may explain why the highest PEP-effected lung function improvements did not translate into higher sputum yield. The PEP method clears more sputum that AD or combination techniques. Patients suffering from airway hyperreactivity should opt for AD, or take premedications with a bronchodilator before using PEP.

Chest Physiotherapy In Cystic Fibrosis: Improved Tolerance With Nasal Pressure Support Ventilation
Pediatrics (1999). 103 (3). e32.
CPT (chest physiotherapy) is an important part of treating patients with cystic fibrosis. Additional respiratory work may be required by CPT, which can lead to respiratory muscle fatigue. Inspiratory pressure support ventilation (PSV) is a new mode of ventilatory assistance designed to maintain a constant preset positive airway pressure during spontaneous inspiration with the goal of decreasing the patient’s inspiratory work. Our research had two goals: to examine respiratory muscle fatigue as well as oxygen desaturation in CPT; and to establish if PSV, which is not invasive, can reduce these adverse CPT effects.
The study involved 16 CF patients with stable conditions and a median age of 13+- 4 years. For CPT, we used the forced expiratory technique (FET), which consisted of one or more slow active expirations starting near the total lung capacity (TLC) and ending near the residual volume. After each expiration, the child was asked to perform a slow, nonmaximal, diaphragmatic inspiration. The child was then asked to exhale and cough after one to four forced breath cycles. CPT consisted in a 20 minute session that included 10 to 15 FET maneuvers, separated by 10 to 20 breath cycles. During the study, each patient received two CPT sessions in random order on two different days, at the same time of day, with the same physiotherapist. During one these sessions, PSV, which was delivered via a nasal-mask using the pressure support generator ARM25 intended for acute patients, was available. The control session had no PSV and was done without a nasal mask. The CPT sessions did not include supplemental oxygen. Prior to and following each CPT session were taken measurements of lung function, maximal inspiratory pressures and expiratory tensions.
Before the PSV, mean lung function parameters were identical to the controls. Baseline pulse-oximetry (Spo) significantly correlated with the baseline vital capability (% predicted) and forced expired volume in 1 second(FEV) (% predicted). PSV was associated a rise in tidal Volume (Vt) between 0.42 + – 0.01 and 1.0 + – 0.02 L. PSV significantly reduced the rate of respiration. PSV session had significantly lower Spo after FET maneuvers than control. The Spo drops after FET decreased significantly more during the PSV sessions (93.8 +– 0.6%) and the control session (91.9 +– 0.7%). Maximal pressures were lower during the PSV, when they increased between 71.9 +-6.9 and 60.9 +-5.3 cmHO, respectively. Pemax decreased significantly was correlated with severity of bronchial blockage as measured by baseline FEV (% expected). The CPT session did not alter the forced expiratory flows. It was identical for both CPT sessions: 5.3 +-5.3 g to 4.6 + 4.8 g (NS) PSV was a session that made fifteen patients less tired. PSV helped expectoration for 10 patients, while 4 patients felt no difference. 2 patients were not able to expectorate. PSV won the preference of nine patients. PSV had a slight preference among five patients. PSV also received some positive feedback from two patients. PSV made CPT easier in 14 of the patients, while 2 patients did not notice any differences.
Our study in CF children shows that respiratory muscle performance, as evaluated based on various parameters, decreased after CPT and that significant falls in oxygen saturation occurred after the FET maneuvers despite the quiet breathing periods between each FET cycle. Noninvasive PSV administered via a nasal mask reduced both these unwanted side effects. Noninvasive PSV delivered via a nasal mask to CF patients partially compensated for increased inspiratory overload due to FET. This may have resulted in a decrease of the inspiratory workload. The patient may be able to focus on their expiratory effort with the help of a physiotherapist. This is key to FET’s efficacy.
Our study showed that Pimax and Pemax were significantly lower after the PSV session. This suggests that CPT may be associated with fatigue in the respiratory muscles. Pimax levels improved markedly after the PSV training. PSV creates an unchanging amount of positive pressure when spontaneous inspiration occurs. It acts as an external inspiratory muscles that decreases effort and oxygen cost. PSV is known to lower diaphragmatic activity, and reduce diaphragmatic fatigue among chronic obstructive-pulmonary disease patients. PSV might “rest” CPT muscles, as shown by our Pimax improvement after PSV. PSV can increase Vt, which could account for the improvements in Pemax. The tendency of the Vt to increase during PSV is the TLC. The Vt tends to the TLC, which allows for more energy to accumulate. This facilitates expiration and decreases the workload of the expiratory muscle.
The beneficial effect of PSV on Spo can be explained by the large Vts, which can improve ventilation-perfusion mismatching.
This is the first study to demonstrate that PSV with nasal masks during CPT can improve respiratory muscle performance as well as reduce oxygen saturation. CPT compliance in CF patients may be improved by a better patient experience. respiratory muscles, lung function, children, cystic fibrosis, oxygenation, inspiratory assistance by positive airway pressure, mucus.
Copyright (c-99 American Academy of Pediatrics) You currently do not have any access to this content.
.Chest Physiotherapy For Cystic Fibrosis
Kent Chiro-Med Wellness Clinic
| Website | https://www.kentchiromed.com/ |
| Address | 563 Gladstone Ave, Ottawa, ON K1R 5P2, Canada |
| Phone | +1 613-508-0113 |
| Category | Physiotherapy Ottawa |
Beverly Physiotherapy
| Website | http://www.beverlyphysiotherapy.com/ |
| Address | 747 Ellice Ave, Winnipeg, MB R3G 0B5, Canada |
| Phone | +1 204-774-8385 |
| Category | Physiotherapy Winnipeg |



















:fill(white)

