Cystic Fibrosis Chest Physiotherapy

A summary of plain language
Chest and chest physiotherapy is better than no chest therapy for cystic-fibrosis
Review question: We reviewed evidence regarding the effectiveness of chest physiotherapy in clearing out excess mucus from cystic fibrosis patients’ lungs.
Background Cystic fibrosis causes excessive mucus production in the lungs. The lungs become infected and can cause tissue damage. It is important to clear the mucus using drugs and chest physiotherapy. The mucus is cleared using either physiotherapy or mechanical equipment. It can take a lot of effort and time to do daily physiotherapy. The studies that showed equal participation in chest physiotherapy and those without it were searched. This revision is a reprint of previous reviews.
Date of search The evidence is up to date as: 02/06/15
Studies that included cystic fibrosis patients were reviewed. Eight studies were selected for the review. There were many studies that looked at several treatments, some compared to none. One research looked at autogenic draining, while six others examined conventional chest physiotherapy. Three other studies considered oscillating negative expiratory pressure. Seventeen considered positive expiratorypressure, and seven evaluated high-pressure positive expiratory. To analyse the data statistically, we could not combine them.
Key results Summarising the findings of these eight studies, we found that methods of clearing the airways have short-term benefits for moving mucus. A total of three studies looked at the amount of sputum coughed up. Three found people who had used chest therapy coughed out more. Four other studies assessed radioactive tracer levels and discovered that chest physiotherapy gave greater clearance. One study did not report an improvement in lung function, while three others reported no significant effects from chest physiotherapy. Chest physiotherapy has not been shown to have any long-lasting effects on survival, chest clearance or quality of living.
Quality of the evidence. Many studies that were included in this review had problems with their design which might have affected confidence. It was unclear whether every result from half the included studies had been reported.
A person’s physiotherapist, and they will both know what treatment they have received in their studies of physiotherapy. These may influence some of the results. The amount of sputum gathered and the results of lung function tests were examined in half of the studies. A quarter of these questions asked the participants their opinions on the treatment. These findings may have been affected if they weren’t aware that the treatment was being used. None of the studies revealed whether the subject was competent in applying the treatment. The ability to perform the treatment may be affected, and this could have an impact on the quality of the results.
Abstract
Although there are no evidence for its regular use, non-cystic fibrosis patients with bronchiectasis recommend that chest physiotherapy be done regularly. This study aimed to establish the efficacy of regular chest physiotherapy in non-cystic fibrosis bronchiectasis compared with no regular chest physiotherapy. Randomized crossover trials were conducted in which 20 patients did not receive regular chest physical therapy. The Leicester Cough Questionnaire, (LCQ) was the primary endpoint. Other outcomes were 24-h sputum volume (FEV(1)), forced expiratory volume (FVC), force vital capacity (FVC), and forced expiratory flow at 25-75 maximum inspiratory (MIP)), maximum expiratory (MEP), exercise ability, and the St George’s Respiratory Questionsnaire (SGRQ). To estimate the effect of treatment, we used the difference between the observations of each patient. With regular chest physiotherapy, there was a marked improvement in all domains (interquartile range) and the total LCQ score (median (interquartile Range) score improvement 1.3 (-0.17-3.25 units; p=0.002). 24-h sputum volume increased significantly with regular chest physiotherapy (2 (0-6) mL; p = 0.02), as did exercise capacity (40 (15-80) m; p = 0.001) and SGRQ total score (7.77 (-0.99-14.5) unit improvement; p = 0.004). The results of sputum bacteria, FEV(1), FVC,FEF(25-75%),MIP and MEP showed no significant difference. Non-cystic fibrosis bronchiectasis sufferers can benefit from regular chest physiotherapy. However, the benefits are not significant.

Abstract
BACKGROUND–Autogenic drainage has been suggested as an alternative method of chest physiotherapy in patients with cystic fibrosis. The autogenic drain was tested against the combination of active breathing techniques (ACBT), and postural drainage. METHODS–Eighteen cystic fibrosis patients participated in an randomised crossover study of two days. The two-day crossover trial involved one session of each method of physiotherapy, autogenic or ACBT. These study days took place one week apart. Patients were monitored every day for six hours. A radioaerosol method was used to measure mucus movement. At the beginning and ending of each day, airway clearance was qualitatively assessed using xenon133 scintigraphic analyses. Each session of physiotherapy included a collection of expectorated stool. This was done for an hour before and after the sessions. Each session was followed by a test of the lungs. Each session was measured for oxygen saturation (SaO2) or heart rate. RESULT–Autogenic Drainage cleared more mucus from the lungs than ACBT during the entire day. Based on the xenon133 ventilation study, both methods significantly improved ventilation. There were no overall differences in the results of the pulmonary function tests. However, more patients showed improved forced expiratory flow (from 25% to 75% with Autogenic Drainage) while more had an increased forced vital capacity with ACBT. Over the course of the series there were no significant differences in heart beat, sputum volume, or mean SaO2. However, ACBT was used to desaturate four patients. CONCLUSIONS–Autogenic drainage was found to be as good as ACBT at clearing mucus in patients with cystic fibrosis and is therefore an effective method of home physiotherapy. Cystic fibrosis patients should be evaluated to determine which treatment is best for them.
Abstract
Objective: CPT is an essential part of treating patients with cystic fibrosis. CPT imposes additional respiratory work that may carry a risk of respiratory muscle fatigue. With the aim of decreasing inspiratory work, inspiratory pressure support ventilation (PSV) is an innovative mode of ventilatory help. This allows for a steady preset positive pressure to be maintained during spontaneous inspiration. This study was designed to 1) evaluate oxygen dehydration and respiratory muscle fatigue during CPT, and 2) determine if PSV is noninvasive and can alleviate the potential negative effects of CPT.
Methods. The study included 16 CF patients who were stable and with a mean age between 13 +/-4 years. CPT used forced expiratory techniques (FET), consisting of one or two slow active expirations, beginning near the total lung capacity and ending at the residual volume. The child was then asked to do a slow diaphragmatic inhalation after each expiration. The child was then asked to exhale and cough after one to four forced breath cycles. CPT sessions lasted between 10 and 15 minutes. Each session included rest periods that spanned 10 to 20 cycles. Two CPT sessions were provided to each patient during the trial. Each session was held on separate days at different times and with the same physician. During one of the sessions, PSV was offered via a nasal support device ARM25 (TAEMA), Antony. PSV was not used in the control session. The CPT sessions did not include supplemental oxygen. Prior to and following each CPT session were taken measurements of lung function, maximum inspiratory pressures (PImax), as well expiratory pressures.
Test results: Lung function parameters for both the PSV session and control were roughly comparable. Baseline pulse oximetry was (SpO2) significantly related to baseline vital capability (% predicted) and forced expiratory flow in 1 second(FEV1) (% predicted). PSV was associated to an increase in the tidal volumes (Vt), from 0.42 +/ 0.05 liters up to 1.0 +/ 0.02 liters. PSV resulted in a significantly decreased respiratory rate. PSV showed significantly greater SpO2 levels between FET maneuvers than in the control sessions. SpO2 declines following FET were more pronounced during the control session (91.8 +/- 0.2%). However, SpO2 decreased significantly after FET (nadir: 91.8+/- 0.7% and 85.3 +/ 7.9 to 77.5 +/- 8.8 cmH2O respectively) than during PSV (83.8 +/ 0.6%). Maximal pressures fell during the PSV-session (from 71.9+/– 6.9 to 60.9+/–5.3 cmH2O et al., 85.3+/– 7.9 cmH2O PImax & PEmax, respectively), and rose during the PSV-session (from 71.6 +/– 8.6 cmH2O to 83.9 +/– 8.7 cmH2O et al., 80.4 +/– 7.8 cmH2O PImax /-max and 8.0 +/–7.4 cmH2O, respectively, PImax /-PEmax PImax /- As measured using baseline FEV1 and % predicated, the PEmax drop was significantly related with severity of bronchial congestion. Both CPT sessions resulted in no change in forced expiratory flows. There was a similar amount of sputum expectedorated between the CPT sessions (5.3/-5.3 g vs. 4.6 +/ 4.8 g following the PSV session; NS). PSV sessions made 15 patients feel less tired. Ten patients reported that expectoration was easier with PSV, whereas 4 did not note any difference; 2 patients did not expectorate. PSV was preferred by nine patients, five of whom indicated a preference. Two patients did not have a preference. PSV and CPT were easier to do in 14 patients. PSV did not make any difference for the 2 remaining patients.
Discussion: We found that CPT had adverse effects on the respiratory muscles of CF children. This was based upon a variety of parameters and showed that oxygen saturation decreased significantly after CPT. These were undesirable effects of CPT.

Similar Articles
Chest physiotherapy can be done with non-invasive ventilation in adult cystic Fibrosis patients who have experienced acute exacerbations.
Holland AE, Denehy L, Ntoumenopoulos G, Naughton MT, Wilson JW. Holland AE, et al. Thorax. 2003 Oct;58(10):880-4. doi: 10.1136/thorax.58.10.880. Thorax. 2003. Article in PMC for free: PMID 14514944 Clinical trial.
Exercise for children suffering from cystic fibrosis: Timing and driving parts of their breathing strategy
Keochkerian D, Chlif M, Delanaud S, Gauthier R, Maingourd Y, Ahmaidi S. Keochkerian D, et al. Pediatr Pulmonol. 2005 Nov;40(5):449-56. doi: 10.1002/ppul.20266. Pediatr Pulmonol. 2005. PMID 16163725 The effects of PEP Mask physiotherapy and flutter on the symptoms and function of children with cystic Fibrosis
van Winden CM, Visser A, Hop W, Sterk PJ, Beckers S, de Jongste JC. van Winden CM, et al. Eur Respir J. 1998 Jul;12(1):143-7. doi: 10.1183/09031936.98.12010143. Eur Respir J. 1998. Clinical Trial. PMID: 9701429
Hachenberg T. Hachenberg T. Anaesthesist. 1996 Sep;45(9):839-55. doi: 10.1007/s001010050319. Anaesthesist. 1996. PMID: 8967603 Review. German.
[Physiopathology for acute respiratory failure (COPD) and asthma]
Mergoni M, Rossi A. Mergoni M, et al. Minerva Anestesiol. 2001 Apr;67(4):198-205. Minerva Anestesiol. 2001. PMID: 11376510 Review. Italian.
Abstract
Background: Chest physiotherapy is widely used in people with cystic fibrosis in order to clear mucus from the airways. This update is a copy of reviews that were previously published.
The objectives of this study were to determine whether chest physiotherapy is more effective and acceptable than spontaneous cough or no treatment for cystic fibrosis.
Search methods: We searched the Cochrane Cystic Fibrosis and Genetic Disorders Group Trials Register which comprises references identified from comprehensive electronic database searches and handsearches of relevant journals and abstract books of conference proceedings.Date of the most recent search of the Group’s Cystic Fibrosis Trials Register: 02 June 2015.
Selection criteria: A randomised or quasi-randomised clinical study in which a method of chest therapy (airway clearance) was used to treat cystic fibrosis patients. This technique is compared with no physiotherapy or spontaneous cough.
Data collection, analysis and assessment: Each author independently assessed eligibility for the study and extracted the data. The authors also evaluated the potential biases in the studies. The published results were heterogeneous, and variable reporting meant that it was impossible to pool the data in meta-analysis.
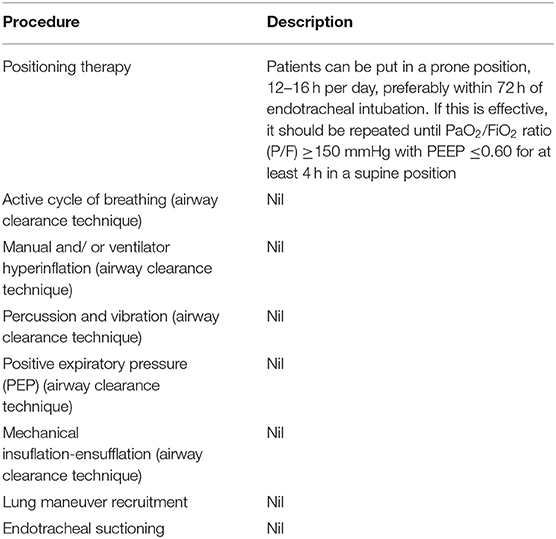
Principal results: There were 157 studies found in the searches. Eight cross-over studies with data from 96 participants met the inclusion criteria. There were differences between studies in the way that interventions were delivered, with several of the intervention groups combining more than one treatment modality. One included study looked at autogenic drainage, six considered conventional chest physiotherapy, three considered oscillating positive expiratory pressure, seven considered positive expiratory pressure and one considered high pressure positive expiratory pressure. Sixteen of eight studies had single treatment. In two studies, the intervention took place over two days. One was twice daily, and the second, once daily. A meta-analysis could not be done due to this heterogeneity. It is not possible to blind participants, caregivers and clinicians during airway clearance studies. Therefore this risk was not considered high. Because of the lack of protocols data, it was difficult to assess risk of bias for most of the criteria. There were four studies that involved 28 participants and reported an increase in expectorated secretions when chest physiotherapy was performed. A single study, which involved 18 participants, found no differences in the sputum weight. As an outcome variable, five of the studies included radioactive tracer clearing. One study (28 participants) reported an increase in radioactive tracker clearance due to chest physiotherapy. A single study, which included 12 participants, reported an increase in radioactive tracer clearing associated with all interventions, but this only reached significance for postural drainage using percussion and vibrations. The remaining eight participants (eight) did not report any significant differences in radioactive tracer cleared between chest physiotherapy and coughing. A total of three studies involving 42 subjects found that intervention did not have a significant impact on lung function. But, one study showed significant improvements in pulmonary function in certain treatment groups.
Conclusions of the authors: This review shows that airway clearing techniques can have short-term results in terms of increasing mucus transportation. There was no evidence to support long-term effects.
Abstract
Background: Cystic Fibrosis can be described as a multisystem disorder. The main issues are in the respiratory system. The best way to increase physical fitness is through aerobic exercise.
This study had one objective: To evaluate the effect of aerobic exercise training and chest physiotherapy on young cystic fibrosis patients.
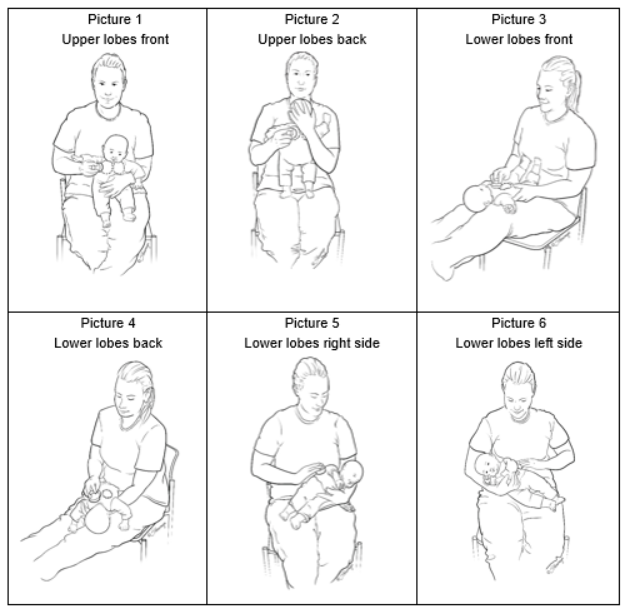
Methods: Sixteen patients with cystic fibrosis, between the ages 5-13 years, were included in this study. All children were assessed at the beginning and at the end of 6 week of the training. To assess cardiovascular endurance, Modified Bruce protocol (or modified Bruce) was used. The standing test, which measures dynamic endurance, was used to examine abdominal muscles. Also, the trunk rotation, trunk hyperextensions, trunk rotation, forward bending, trunk tilt, and trunk lateralflexion tests were used. A 20-m shuttle run test, as well as 10-step stair climb tests, were used to check agility and power. For six weeks, all patients were treated with chest physiotherapy as well as aerobic training three days per week. A treadmill-based aerobic exercise and active breathing program were used.
Results: By evaluating the results of the training, positive progressions in all parameters except 20 m shuttle run and 10 stairs climbing tests were observed (p < 0.05). An active cycle with breathing techniques and exercise training were combined in patients suffering from clinically stable cystic fibrillis. This increased thoracic mobility (p0.05), and physical fitness parameters (p0.05). Comparison of the results in sit and reach and forward bending tests were not significant (p > 0.05).
Conclusion: In addition to medical treatment, it is believed that the active breathing cycle and aerobic training help to increase the aerobic capacity, thoracic mobility, as well as physical fitness, in children suffering from cystic fibrosis.
Abstract
BACKGROUND–Autogenic drainage has been suggested as an alternative method of chest physiotherapy in patients with cystic fibrosis. Autogenic drainage was studied in conjunction with ACBT and postural drainage. METHODS–Eighteen sufferers with cysticfibrosis were randomly assigned to a crossover two-day trial. On each day, there were two sessions of either autogenic drain or ACBT physiotherapy. One week separated the study days. On each day the patients were monitored for six hours. Mucus movement was quantified by a radioaerosol technique. A radioaerosol technique was used to measure airway clearance. This method was done at both the beginning and ending of each day. Expectorated sputum was collected during and for one hour after each session of physiotherapy. Every session included a pulmonary function test. Before, during and after every session, oxygen saturation (SaO2), heart rate, and blood pressure were all measured. Results–Autogenic draining cleared the lungs of mucus quicker than ACBT throughout the day. According to the xenon133 ventilation tests, both methods resulted in better ventilation. No overall differences were found in the pulmonary function test results, but more patients had an improved forced expiratory flow from 25% to 75% with autogenic drainage, while more showed an improved forced vital capacity with ACBT. In the series of pulmonary function tests, there was no variation in sputum, heartbeat, or mean SAO2 but ACBT desaturated four patients. CONCLUSIONS–Autogenic drainage was found to be as good as ACBT at clearing mucus in patients with cystic fibrosis and is therefore an effective method of home physiotherapy. Cystic fibrosis patients should be evaluated to determine which treatment is best for them.
.Cystic Fibrosis Chest Physiotherapy
Kent Chiro-Med Wellness Clinic
| Website | https://www.kentchiromed.com/ |
| Address | 563 Gladstone Ave, Ottawa, ON K1R 5P2, Canada |
| Phone | +1 613-508-0113 |
| Category | Physiotherapy Ottawa |
Beverly Physiotherapy
| Website | http://www.beverlyphysiotherapy.com/ |
| Address | 747 Ellice Ave, Winnipeg, MB R3G 0B5, Canada |
| Phone | +1 204-774-8385 |
| Category | Physiotherapy Winnipeg |



















:fill(white)

